The Postbac Premed Program offers a great opportunity to get hospital experience: the Lahey Clinical Research Preceptorship program. Applications for this year’s preceptorships are due on August 16. T. Howell Burke reflects on his past year working at Lahey:
Here is my advice to anyone enrolled in the post-baccalaureate premedical program: get out of the library! The skills in problem-solving and basic science you will learn in chemistry, physics, and organic will help you on the MCAT and will be important to your career as a healthcare professional, and the labs can even be fun sometimes.
However, you will eventually be working in a hospital, not a lab or classroom – so take any opportunity you can to get into a hospital. Clinical experience is an important part of the discernment for a medical career, and it is also a lot of fun.
During my second year in the Tufts Postbac Program, I had the opportunity to participate in the preceptorship at Lahey Hospital in Burlington, MA. My advisor, Edwin Ozawa MD PhD, is one of the more impressive people I have met: he had a career in bioengineering before he became an anesthesiologist. As an engineer, he is constantly tinkering with systems – including the way that specialized teams of anesthesiologists, pharmacists, and nurses at Lahey respond to code blue events, in which a patient goes into cardiopulmonary arrest.
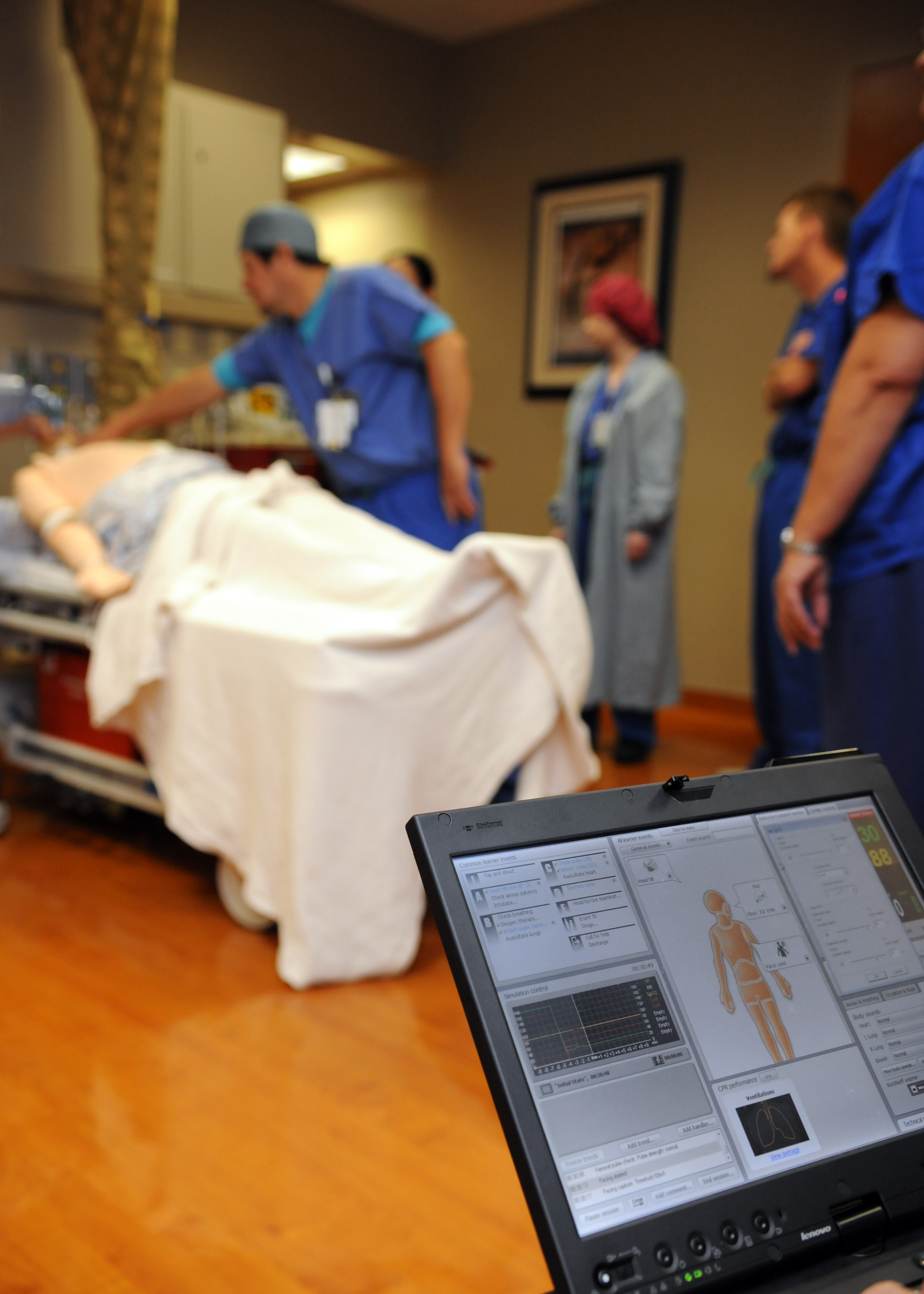
Dr. Ozawa was looking for help improving the response of code blue teams to such events. We designed and ran simulated code blue events using the SimMan 3G, a sophisticated $100k electronic mannequin that could simulate a lot of human physiology (it could even talk). The clinical management and teamwork of code blue teams during these simulated events were scored using an evaluation tool that I designed.
This work required that I have a working understanding of code blue pathology and clinical management. I spent a lot of time reading American Heart Association algorithms, analyzing video of simulated code blue events, and even observing real code blue events. “Grading” MDs on their clinical skills definitely felt strange, but it is what I was asked to do!
A laptop is used to control a training mannequin’s vital signs during a mock code blue drill at the pain management clinic at Naval Medical Center San Diego. (U.S. Navy Photo by Mass Communication Specialist 1st Class Anastasia Puscian/Released)
The position was also a great opportunity to form a close working relationship with a physician that I respect. Dr. Ozawa and I spent many hours discussing our mutual interests in naval history, military strategy (he is a reservist with the U.S. Navy, and I am applying for the U.S. Navy medical scholarship), teamwork behavior, and Legos (nerd alert, people). The mentor relationship drives medical education and training, and I feel fortunate that I can count Dr. Ozawa among my mentors.
While I probably will not pursue anesthesiology as a specialty, my work at Lahey did get me interested in the details of critical care, including airway management, as well as the human systems underlying emergency management, skills which are important in other medical specialties that I am interested in pursuing.
You might have heard the cliché that medicine is a career of lifelong learning. My experience at Lahey demonstrated the truth of this cliché: physicians decades into their careers were eager for additional opportunities to train and fine-tune the way they responded to critical care events. I feel fortunate to be included in such a group.
Leave a Reply