My Sites
Log in to create or edit your sites.
IMPORTANT SERVICE ANNOUNCEMENT: Content freeze 7am June 19th until 7am June 23rd. Read more here.
Need Help? Email edtech@tufts.edu
Site-Wide Activity
-
Kyle Slinger wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
-
Jacob Rosenberg wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
-
Christopher Rodriguez wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
-
Michael Nuzzolo wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
-
Riley J. Baldwin is attending Seminar V. 10 years ago
-
Jennifer E. Wilson is attending Seminar V. 10 years ago
-
Nicholas M. Boschetti is attending Seminar V. 10 years ago
-
atiruv01 is attending Seminar V. 10 years ago
-
Tegan Kehoe wrote a new post on the site Museum Studies Blog at Tufts University 10 years ago
Thursday, March 26, 6pm
Hosted by the Peabody Museum of Archaeology and Ethnology, at the Geological Lecture Hall, 24 Oxford Street Cambridge, MA.
Donald J. LaRocca, Curator, Department of Arms and Armor, […]
-
lcekal01 is attending Seminar V. 10 years ago
-
Huy Nguyen is attending Seminar V. 10 years ago
-
Katherine Levinson wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
Robotic Assisted Surgery
Abstract
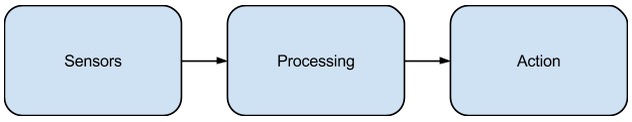
Robotic assisted surgery is one of the newest areas of innovation in minimally invasive surgery. Robots used in surgery offer the potential for safer and more easily repeatable surgeries, minimizing the risk to the patient. Surgical robots can be broken down into two categories: active and passive. Active robots are autonomous, while passive robots require more interaction from the surgeon or user. This article briefly reviews some of the current technology used for passive and active robotics.Introduction
Robots used for surgery offer the potential for safer and less invasive procedures to be performed. A surgical robot may be set up next to the surgeon to assist, or may eliminate the need of a surgeon in the operating room altogether. Many of the types of surgical robots listed below are the newest developments in minimally invasive surgeries. Compared to open surgeries, during minimally invasive surgeries the surgeon performs the procedure with less injury to the body. This allows the patient to heal faster, and decreases the risk of infection. Some of the downsides of minimally invasive surgeries are the high cost of the tools, and the training required so that surgeon may use these tools (Sobh & Xiong, 2012).The first non-robotic minimally invasive surgery technique was the laparoscopic approach and is often called the “zeroth” generation of robotic surgery. Laparoscopy is the process by which access to the pathology location is gained through small incisions made in the abdominal cavity. An elongated tool is inserted into each of the incisions, and an endoscopic camera is inserted into one of the incisions as well. Depending on the type and complexity of the surgery, three to six ports are typically used (Bergeles & Yang, 2014).
The advantages of laparoscopic surgery include an expedited recovery time for the patient, decreased risk of infection, and less stress on the patient’s body; however, laparoscopy is limited in its abilities. The endoscopic camera used in laparoscopic surgery does not give a stereoscopic view, which provides surgeons with depth perception. In addition, hand-eye coordination that surgeons are used to during open surgery is gone because their hands are outside of the patient. Finally, the tools do not have the same degrees of freedom of movement that a wrist does. Surgical robots strive to restore these missing aspects and improve upon laparoscopic surgery.
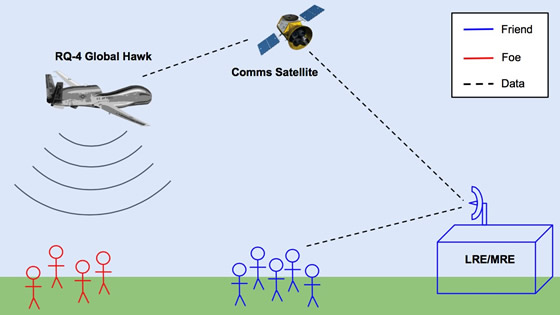
Developments in electrical and computer engineering have allowed for the possibility of advancing and developing surgical robots, a new field of minimally invasive surgery. Because surgical robots can be sterilized and have more precision than humans, they offer the potential to decrease the risk during surgery and of post-operative complications for the patient. Another advantage of robotic surgery is the potential for tele-surgery, where the surgeon is in a different location than the robot. This could be used in military applications, so surgeons could remotely and safely operate on wounded soldiers (Hussain & Malik, 2014).
The field of surgical robotics can be broken down into passive and active robots. Active robots are defined to autonomously perform surgeries, and they require little to no intervention by the surgeon. Passive robots are unable to perform surgery without the intervention of a surgeon. Passive robots are often used to define a surgical entry path or specifically to increase the surgeon’s accuracy and precision (Bergeles & Yang, 2014). Below, a brief survey of several passive surgical robots will be discussed, followed by a discussion of active robots.
Passive Robots
The first passive robot was called the PUMA 200 and was used to define the entry orientation and location of a surgical needle, and then turned off while the surgeon performed the rest of the surgery (Bergeles & Yang, 2014). The PUMA 200 gave surgeons within one-millimeter precision when defining the entry orientation and location of the surgical needle, much more precise than a trained surgeon can achieve. A later but similar robot, called the NeuroMate, was developed for use exclusively in neurosurgeries (Bergeles & Yang, 2014). This type of passive surgery works well with neurological and orthopedic surgeries as opposed to soft-tissue surgeries. From patient to patient, the structure of the skull and skeletal system does not change dramatically, thus a positioning robot can translate easily.One of the most popular categories of passive robots is the hand-held robot because they are the most similar to the tools surgeons are used to. Hand-held robots can be broken down into five major categories. Tremor suppression devices can detect their own motion and filter out erroneous motion. They then cause the surgical end-effectors to compensate for this motion. This is a tool often used in microsurgery, such as retinal surgery. In order to be able to accurately detect a wide range of motion, the device needs to have a high bandwidth – a problem that can be solved with the use of electrical and computer engineering (Payne & Yang, 2014). One device that has been implemented as a hand-held tremor suppression device is the Micron. The Micron was intended for use in microsurgeries, especially retinal surgery. It actuates its own tip to cancel tremor. Because it is a hand-held mechanically ungrounded device, the Micron only preserves 1:1 force feedback, meaning that the force exerted on the tool can be directly felt by the operator. In microsurgeries, such as retinal, it would be valuable to have a scaled force feedback because the tool tip is so small and the tissue is so soft. Implementing this in mechanically ungrounded devices is still an ongoing area of research (MacLachlan et al., 2012).
Another type of hand-held device is guidance systems, which are used to constrain tool motion and are often used in conjunction with image guidance systems. They can constrain a surgical tool toward or away from a pre-defined point. For example, the NavioPFS is used for partial knee replacement. The cutting tool is retracted when the constraint boundary is approached, so the surgeon does not cut too deep (Payne & Yang, 2014). One advantage of the NavioPFS is that it has planning and robotics-assisted bone-preparation embedded into the device, so the surgeon can make a more precise surgical plan because of the added information fron the NavioPFS (Gregori, Lethbridge, & Simone, 2013). However, as with many of these new surgical robotics, the NavioPFS does have a learning curve. It was found that on average it took surgeons eight procedures to reach two out of three consecutive cases within a 95% confidence interval (Wallace et al., 2014).
The third type of hand-held device is the articulated mechatronic device, which is used to help restore dexterity to the surgeon. The Laparo-Angle is used in laparoscopic surgeries and uses motor actuation to articulate the tip of a laparoscopic tool to control roll, yaw, and triggering functions. The surgeon is able to achieve seven degrees of freedom, which makes positioning and controlling the device easier and makes the device feel more natural. However, by adding various controls that make the Laparo-Angle function more as a surgeon’s hand would, it has added complexity to the device and lengthened the learning curve (Rao, Rao, Bhagwat, 2011).
A fourth type of hand-held device is the force control systems, which are used for active tool-tissue contact stabilization, especially in beating heart surgery. Yuen et al. (2009) developed a mechatronic force control device to be used in beating heart surgery, which can deal with the periodic motion of the heart and a high bandwidth. This device uses force control of the instrument against the surgical target. In addition, it feeds forward tissue motion information generated by real-time 3D ultrasound, improving the performance of the force controls (Yuen et al., 2009).
Finally, haptic feedback devices use force sensing and integrated actuation to provide force-feedback. Hand-held devices inherently provide haptic feedback because the surgeon handles them, but the goal is to enhance tool-tissue interactions (Payne & Yang, 2014). For example, the MicroTactus developed by Yao et al. (2005) senses tool-tissue interactions with an accelerometer and a magnetic actuator. The magnetic actuator amplifies the signals from the accelerometer to provide vibrotactile feedback to the surgeon. This allows the surgeon to get a better sense of the surface they are dealing with, and cuts or surface patterns that may exist. One problem that still needs to be addressed for this device is that the amount of gain, or amplification, in the system was limited, so it would be unable to detect the smallest of signals (Yao Hayward, & Ellis, 2005). Passive robots offer surgeons improved performance while keeping the surgical instruments as close to traditional tools as possible.
Active Robots
The first active robot developed was the ROBODOC, which works in conjunction with the ORTHODOC. This robot acquires a CT scan in order to develop a surgical plan, and then autonomously performs the surgery. The only time the surgeon intervenes is to overlook the surgical plan and make any necessary changes (Bergeles & Yang, 2014). These two robots are used for orthopedic surgeries, specifically for total joint replacement. The ORTHODOC acquires the CT scan, and converts it to a 3D bone image. This allows surgeons to look at different implants and positions for the implant so the best option can be selected for the patient. The ROBODOC then drills into the bone with sub-millimeter accuracy, as defined by the ORTHODOC’s plan (“Transforming Total Joint Replacement with Active Robots”).A study comparing the use of the ROBODOC/ORTHODOC versus a manual hand-rasping technique during the implantation of a cementless total hip arthroplasty found some advantages to the robotic approach, but with more generally mixed results (Nakamura, Sugano, Nishii, Kakimoto, & Miki, 2010). For example, one year after the operation only 1.3% of patients with the robotic surgery complained of thigh pain, compared to 5.6% of patients with the manual surgery. In addition, the limb-length inequality was found to be on average 5mm in the robotic patients, and closer to 6mm in the manual patients. Interestingly, the robotic method took approximately 120 minutes while the hand-rasping method took only approximately 108 minutes. The number of post-operative hip dislocations was seen in 5.3% of the patients who underwent the robotic surgery, and only in 1.4% of the patients who underwent the hand-rasping method. Clearly, while the ROBODOC is not a flawless method of surgery, it does offer potential for making orthopedics surgery more consistent and safer (Nakamura, Sugano, Nishii, Kakimoto, & Miki, 2010).
One of the most popular active robots is called the daVinci. The daVinci is considered a tele-operated robot, meaning the surgeon is able to remotely control a patient-side slave robot through manipulation of the master manipulator (Yang, Wang, Liu, & Wu, 2013). While the ROBODOC and ORHTODOC are used primarily for orthopedic surgeries, the daVinci is used for a range of surgeries, including cardiac, colorectal, general, head and neck, thoracic, and urological surgeries. The daVinci has two main units; the first is the surgeon’s control unit. This houses the display, the surgeon’s user interface, and the electronic controller. The second unit has four slave manipulators, or essentially arms. Three of these arms are for telemanipulation and have the tools to perform the surgery, while the fourth has an endoscopic camera for visualization (Freschi et al., 2013).
One of the advantages of the daVinci is that the surgeon operates with their gaze towards their hands, which helps restore their hand-eye coordination. In addition, the arms have seven degrees of freedom in order to more accurately mimic a surgeon’s hand movement. The endoscopic camera is a 3D endoscope with two separate optic channels, connected to a pair of charged-coupled device chip cameras. The optic channels are separated by 6mm, creating a true stereoscopic image. This significantly helps the surgeon with orientation and manipulation. In addition, the images are filtered to eliminate noise, and are displayed on high-resolution monitors (Yang, Wang, Liu, & Wu, 2013). These advances in the field of optics and image processing fall into the category of electrical and computer engineering. While these technologies present the surgeon with a more realistic surgical field, the daVinci still lacks haptic feedback (Bergeles & Yang, 2014).
One of the newer fields in robot surgery is that of untethered microsurgeons. These include capsule endoscopes, which are a millimeter device that can be used to explore the GI tract. The capsule is passively propelled by peristalsis in the GI tract, and can be used for imaging as it moves along. This can assist doctors in making more accurate diagnoses, without invasive procedures. Other capsules have the ability to navigate their way using on board locomotion, some external energy transfer, or possible magnetic steering. One challenge is that the technique used for imaging must be small enough to fit inside the capsule. Endoscopy is orders of magnitude too large, so a different method must be employed. An MRI can verify the placement of the capsule because the magnetic microrobot would appear in the MRI as a detectable artifact. Active robots have the potential for decreasing human error during surgery by adding a precise and accurate interface between the surgeon and patient.
Conclusion
Whether robotic surgery is better than traditional surgery depends heavily on the patient, and the surgery they need. However, surgical robotics have come a long way from where they started, and continue to open doors to less invasive procedures. Many of these advancements have been thanks to both electrical and computer engineering, as well as the computer science needed to control them, and the mechanical engineering required to create the machines. As for the electrical and computer engineering, digital image and signal processing is required for the imaging, as well as an understanding of optics required creating the stereoscopic view. Since these are robots, a heavy level of circuitry is required to create them. As these aspects of electrical and computer engineering continue to advance, so will the field of surgical robotics, making robot assisted surgery increasingly prevalent.
BibliographyBergeles, C., & Yang, G.-Z. (2014). From passive tool holders to microsurgeons: safer, smaller, smarter surgical robots. IEEE Transactions on Bio-Medical Engineering, 61(5), 1565–76. DOI: 10.1109/TBME.2013.2293815
Freschi, C., Ferrari, V., Melfi, F., Ferrari, M., Mosca, F., & Cuschieri, A. (2013). Technical review of the da Vinci surgical telemanipulator. The International Journal of Medical Robotics + Computer Assisted Surgery : MRCAS, 9(4), 396–406. DOI: 10.1002/rcs.1468
Gregori, A., Lethbridge, R., & Simone, A. (2013). Case Study: Totals Aren’t Always an Inevitability. Retrieved from http://bluebelttech.com/products/navio/research-results/. Available at http://bluebelttech.com/site/wp-content/pdfs/Case_Study_Totals_Arent_Always_An_Inevitability.pdf
Hussain, A., Malik, A., Halim, M. U., & Ali, A. M. (2014). The use of robotics in surgery: a review. International Journal of Clinical Practice, 68(11), 1376–82. DOI: 10.1111/ijcp.12492
MacLachlan, R. A., Becker, B., Tabares, J. C., Podnar, G., Lobes, L., & Riviere, C. (2012). Robotics Institute: Micron: an actively stabilized handheld tool for microsurgery. Retrieved from https://www.ri.cmu.edu/publication_view.html?pub_id=7422&menu_code=0307. DOI: 10.1109/TRO.2011.2169634
Payne, C. J., & Yang, G.-Z. (2014). Hand-Held Medical Robots. The Journal of the Biomedical Engineering Society. DOI: 10.1007/s10439-014-1042-4
Rao, P. P., Rao, P. P., & Bhagwat, S. (2011). Single-incision laparoscopic surgery – current status and controversies. Journal of Minimal Access Surgery, 7(1), 6–16. PMCID: 3002008
Sobh, T., & Xiong, X. (2012). Prototyping of Robotic Systems – Applications of Design and Implementation. IGI Global. OCLC WorldCat Permalink: http://www.worldcat.org/oclc/894718325
Wallace, D., Gregori, A., Picard, F., Bellemans, J., Lonner, J., Marquez, R., … Jaramaz, B. (2014). The Learning Curve of a Novel Handheld Robotic System for Unicondylar Knee Arthroplasty. Bone & Joint Journal Orthopaedic Proceedings Supplement, 96-B(SUPP 16), 13. Retrieved from http://www.bjjprocs.boneandjoint.org.uk/content/96-B/SUPP_16/13.abstract
Xu, Y., & Wang, H. (2014). Image processing based surgical navigation system building. In 2014 IEEE Workshop on Electronics, Computer and Applications (pp. 991–994). IEEE. DOI: 10.1109/IWECA.2014.6845789
Yao, H.-Y., Hayward, V., & Ellis, R. E. (2005). A tactile enhancement instrument for minimally invasive surgery. Computer Aided Surgery : Official Journal of the International Society for Computer Aided Surgery, 10(4), 233–9. DOI: 10.3109/10929080500230403
Yang, R., Wang, Z., Liu, S., & Wu, X. (2013). Design of an Accurate Near Infrared Optical Tracking System in Surgical Navigation. Journal of Lightwave Technology, 31(2), 223–231. DOI: 10.1109/JLT.2012.2227943
Yuen, S. G., Yip, M. C., Vasilyev, N. V, Perrin, D. P., Del Nido, P. J., & Howe, R. D. (2009). Robotic Force Stabilization for Beating Heart Intracardiac Surgery. Medical Image Computing and Computer-Assisted Intervention : MICCAI … International Conference on Medical Image Computing and Computer-Assisted Intervention, 5761(2009), 26–33. DOI: 10.1007/978-3-642-04268-3_4
Suggested Reading
See also (Links to other SHP articles):Lenk, Will
-
Amanda Samuels changed their profile picture 10 years ago
-
Andrew Carp wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
-
Sean Cunningham wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
-
William Lenk wrote a new post on the site Electrical and Computer Engineering Design Handbook 10 years ago
Abstract
Rapid developments in wireless technologies have ushered in a new era of medical devices that are improving patient quality-of-life and lowering costs for both healthcare providers and owners. Diagnostic, monitoring, and treatment systems are becoming wearable and implantable, which give them numerous advantages over bulky medical equipment. However, the wireless connectivity and programmability of these devices and applications creates an enormous vulnerability that can be exploited by malicious hackers. This paper will discuss the advantages of wireless mobile medical devices in terms of both functionality and efficiency, presenting examples to support the claim. It will then transition to assess the diversity and severity of security threats inherent to these devices. Finally, current research on potential security solutions will be presented.Introduction
Rapid developments in electrical engineering disciplines such as flexible electronics and miniaturized, wireless technologies have ushered in a new era of medical devices that are improving the quality of life for patients suffering from a wide variety of afflictions. Diagnostic, monitoring, and treatment systems are becoming portable, wearable, and even implantable, which give them numerous advantages over bulky medical equipment, including minimized patient discomfort and lower costs for both healthcare providers and owners. However, the wireless nature of these electronic biomedical devices presents a new set of concerns from previous generations of medical equipment. The main concern regarding wireless operation of these devices is an enormous security vulnerability that can be exploited by malicious hackers. This paper will discuss the advantages of wireless mobile medical devices in terms of both functionality and efficiency, presenting examples to support the claim. It will then transition to assess the diversity and severity of security threats inherent to these devices. Finally, current research on potential security solutions will be presented.
Advantages of Wireless Mobile Medical Devices
As analog and digital electronics become increasingly fast with ultra-low power consumptions, miniaturized electronic systems are becoming viable in previously uninhabitable markets. One market that shows huge potential is the medical space. With micro-sized, ultra-thin, flexible, and biocompatible electronic systems being developed at leading research institutions and corporations, a new era of medical care is burgeoning. Biomedical devices that previously required bulky read-out equipment, large assortments of wires, and importable displays are giving way to wearable and implantable devices that can achieve the same functionality at greatly reduced patient discomfort. In addition, wireless medical solutions are often much more affordable for patients and lower cost for healthcare providers.
Bluetooth Low Energy and other Wireless Protocols
A crucial aspect of this technological shift is the ability to achieve reliable wireless communications with biomedical devices at very low power consumptions, such that the devices can be remotely operable and data can be remotely accessed. Bluetooth technologies epitomize recent advances in wireless technologies that allow for the remote operation of mobile medical devices. In 2010, Bluetooth released its latest wireless platform: Bluetooth Low Energy (BLE), aimed at creating wireless applications in numerous fields including healthcare. The intention of BLE is to provide devices with wireless communications at aggressive power metrics and low costs without sacrificing performance relative to other wireless standards. Table 1 summarizes the relevant performance specifications of BLE chipsets that make them suitable for wireless medical devices.
Table 1
Bluetooth Low Energy Specifications. Source: Bluetooth 4.0: Low Energy (2010, p. 8).Parameter
Value
UnitOpen Field Transmission Range
150
mOutput Power
10
dBmMax Current Draw
15
mASleep Current
1.0
μACarrier Frequency
2.4
GHzData Throughput
1.0
MbpsThe transmission range, output power, and power consumption are all outstanding, making BLE a suitable wireless protocol for use in wireless mobile medical platforms. The sacrifice for achieving transmission at such low power is the limit in data throughput – 1 Mbps (Decuir, 2010). However, the data rate is sufficient for achieving reliable discrete data transfers, such as those required for transmitting data from a sensor node in a biomedical application. BLE systems are designed to run for years on standard 3-volt coin cell batteries, eliminating the concern of constant power-supply replacement for a wearable or implantable medical device (ibid). BLE is just one of many wireless protocols that work reliably at low power consumptions. The use of ANT, ZigBee, and other wireless communications standards are also being explored for use in the medical space. Furthermore, the “internet of things” gives the mobile medical space much more viability in a complex healthcare system: wireless devices can autonomously update electronic medical records by connecting to the internet themselves, or by transmitting data to an internet capable device such as a computer or a smart phone.
Examples of Wireless Mobile Medical Devices
To achieve patient diagnosis, monitoring, and treatment, medical devices from previous generations require probes and sensors which attach to the patient with long wires leading off the probes to a bulky, non-portable display / user interface. The wires and bulky nature of the devices tether the patient to a hospital bed, during which their hospital visits are expensive and in many cases unaffordable. The technology of these generations simply did not allow for wireless mobile medical devices to compete with the performance of cumbersome, importable medical systems. But with the aforementioned advances in electrical engineering, in particular in wireless communications, research-level prototypes for wireless mobile medical devices are emerging across all sectors of medicine. Examples of autonomous wearable or implantable medical devices that are already being employed in the field include pacemakers, defibrillators, glucose monitors, insulin pumps, and neuro-monitoring systems. But this is just the beginning; researchers are working to develop the next generation of wireless medical devices that will revolutionize healthcare on all fronts.
Current Research: Smart Wound Dressing
One example of promising research that combines the use of miniaturized sensor systems, microprocessors, and low-power wireless communications in a biomedical application is an intelligent wound dressing platform. Researchers at Tufts University, Purdue University, and Harvard University are developing a wearable bandaging with integrated sensors, read-out electronics, and wireless communications that can autonomously monitor the process of a healing wound. An early stage prototype was created over the summer of 2014: a wireless flexible smart bandage for continuous monitoring of wound oxygenation (Mostafalu, 2014). Embedded in the bandage is an oxygen sensor as well as an electronic readout system with wireless data transmission for autonomous, real-time, remote monitoring of oxygen concentration at the wound site. Figure 1 shows a 3D rendering of the smart wound dressing, which serves as an exemplary template for wearable medical technologies.
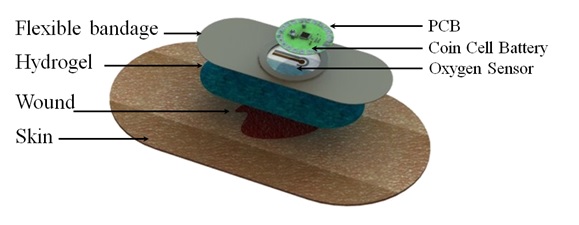
Figure 1
3D Rendering of Wearable Smart Wound Dressing. Source: Wireless Flexible Smart Bandage for Continuous Monitoring of Wound Oxygenation (2014).
A flexible, galvanic oxygen sensor on the order of 100 μm in diameter with a highly linear sensitivity was fabricated and integrated into the bandage (ibid). The oxygen sensor is interfaced via a flexible conductor to an analog-front-end circuit for amplification (ibid). The front end circuit contains a fully programmable, variable-gain, trans-impedance amplifier, allowing for monitoring of a wide variety of oxygen concentrations with oxygen sensors of various sensitivities (ibid). The output of the analog-front-end is read into a microcontroller through an analog-to-digital converter, where the data is converted back to a voltage value and wirelessly transmitted to a nearby computer or smartphone via a Bluetooth Low Energy radio (ibid). Once the data is captured to the smart phone or computer, it can, of course, be uploaded to a server for remote access by a caregiver or physician. The sensors and readout electronics are assembled in a conformal packaging that is sufficiently compact to be embedded in a wearable bandage without causing discomfort to the user. Furthermore, the entire configuration is powered by a single 3-volt coin cell battery (ibid). The smart bandage demonstrates the imminent arrival of wireless medical diagnostic and therapeutic tools that are wearable or implantable across a multitude of healthcare domains.
Security Risks of Wireless Mobile Medical Devices
Mobile medical devices are advantageous for both healthcare providers and recipients. Patients can reduce the burden of frequent hospital visits and bulky medical equipment tethering them to hospital beds, while the cost of care is dramatically reduced for both hospitals and patients. But for all these advantages, the security risks presented by wireless mobile medical devices are significant. A typical mobile medical device will have a low-power wireless communications system, such as a BLE or ZigBee radio. The use of low power radios requires an intermediate base station in close proximity to the user (e.g. 150 meters maximum for BLE) where data can be dumped and subsequently uploaded to a “secure” server through a wireless network such as Wi-Fi. The transmission of data across a wireless network presents a glaring security vulnerability if malicious hackers can penetrate the network security and gain access to confidential patient information. Furthermore, if the medical device itself can directly be accessed or programmed from a remote location, such as the previously discussed smart wound dressing, malicious hackers could actually hijack operation of the device to steal private information or cause device malfunction.
Flavors of Security Breaches
Rushanan et al. break the variety of security threats for implantable medical devices (IMD’s) into three general categories: telemetry interface breaches, software threats, and hardware / sensor threats (Rushanan, 2014). The most commonly considered and most feasible security vulnerability is the telemetry interface. Usually, a wireless network requires knowledge of a network identifier to access the information communicated through the network, much the way many Wi-Fi networks require a password for admittance. If a remote adversary could somehow infiltrate the wireless network by obtaining the network identifier or through other network vulnerabilities, the adversary can pose threats in one of two forms: passive and active (ibid). A passive adversary will eavesdrop on information from the medical device, which compromises patient confidentiality and privacy (ibid). An active adversary can jam, modify, or forge the information exchange, corrupting the data readout from the medical device, or even terminate wireless access to the device altogether (ibid). Active adversaries compromise confidentiality and privacy like a passive attacker, but also threaten the integrity and safety of the medical device. Malicious hackers can also pose more immediate threats to the medical device if they are within range of its remote operation. Familiarity of the embedded software of an IMD would allow the adversary to alter the logic and functionality of the device without having to establish physical contact (ibid). Furthermore, knowledge of the hardware and sensor structure of an IMD would enable an attacker to potentially introduce remote interference that directly compromises sensor operation, sensor read-out, and actuation of treatment (ibid).
How to Breach a Wireless Insulin Pump, For Dummies
Jerome Radcliffe outlines a shockingly feasible scenario in which a wirelessly operable insulin pump using supervisory control and data acquisition (SCADA) could be breached and in turn used for malicious purposes (Radcliffe, 2011). SCADA refers to any system sending coded signals over a wireless communications channel for sensing and actuation, such as those utilized in wireless mobile medical devices. The frequency of wireless communication for the insulin pump in this theoretical attack (916.5 MHz) and the modulation scheme used for wireless transmission from the device (On / Off Keying) is readily available information provided by the device manufacturer (ibid). There are myriad wireless chipsets available in commercial markets that broadcast across all frequency ranges and are programmable to allow for various modulation types, meaning they could be programmed to communicate with this insulin pump. These include wireless radios utilizing the protocols previously discussed (Bluetooth, ZigBee, etc.). In this scenario, Radcliffe used the CC1101 radio transceiver from Texas instruments (TI), which can be directly purchased from TI’s website or through a third party distributor such as Digi-Key. The command codes for wireless operation of the medical device were found to be published in multiple online locations, though not released directly by the insulin pump manufacturer (ibid). The indirect availability of this information calls into question the intentions of those who made it publicly available. Additionally, a dedicated attacker could purchase the same insulin pump and likely gain the necessary knowledge to stage an effective attack through the information provided with the product. Thus the relevant information and hardware needed to hack this insulin pump would be readily accessible to an adversary. With this information, Radcliffe postulates many serious threats, including the ability of the adversary to change the amount of insulin delivered by the pump to the patient (ibid). Although this would require close proximity to the device (100 to 200 feet for the wireless transceiver used on this insulin pump), it would only take seconds to reprogram its functionality, which could potentially result in patient hospitalization or even fatality (ibid).
Security Solutions for Wireless Mobile Medical Devices
If innovation in electrical engineering has enabled the feasibility of mobile medical devices, in turn generating a new set of security risks, then advances in electrical engineering and related fields such as computer science can certainly mitigate these risks as well. Researches are investigating highly advanced data encryption methods, security protocols, and trust models to help secure wireless medical instruments.
Example: Architecture for Trustworthy Data Collection from an IMD
Hu et al. used a public-key cryptography standard—IEEE 1363—in combination with a complex, probabilistic trust model to demonstrate highly trustworthy data collection from IMD’s (Hu, 2010). Public-key cryptography is a scheme in which data is scrambled, or encrypted, such that it is undecipherable in its raw form. To convert the data back to the original, discernable form, two “keys” are required—one public key and one private key. A key can be thought of as an operation which is applied to the encrypted data which uniquely produces the original, unencrypted information. The private key is mathematically related to the public key, but the mathematical relationship will typically not have a closed-form solution, so an adversary obtaining the private key from the public key is neither trivial nor likely—in fact, it is said to be computationally infeasible. <pFurthermore, in this study, a trust model was developed to quantify the level of trust for any user trying to access information through the wireless network (ibid). Instead of using a conventional binary trust quantifier, where the number 1 represents a trusted user and 0 represents an untrustworthy user, Hu et al. used a complex probabilistic framework based on numerous variables to map the level of trust to any decimal on the continuous interval form 0 to 1 (ibid). Based on the encryption scheme and the novel trust model, a protection system was implemented in hardware and shown to be highly effective against a variety of staged attacks ranging from naïve to advanced in nature (ibid). Hu et al. thus demonstrate how encryption algorithms and probabilistic models can be mapped to functionalized electronic systems to secure medical devices. This is just one example of a multitude of research efforts within the electrical engineering discipline that are intended to mitigate the vulnerabilities of wireless medical devices.
Conclusion
In summary, developments across many electrical engineering disciplines have given rise to a new generation of medical devices, ranging from diagnostic to therapeutic, that are wirelessly operable. Wireless functionality reduces patient discomfort, reduces costs for both patients and health care providers, and in many cases improves the efficacy of treatment relative to medical instrumentation from previous generations. At the heart of wearable and implantable medical devices are advances in wireless communications, specifically the ability of wireless radios to achieve sufficient data throughput with ultra-low power consumption on highly miniaturized electronic chips. A typical mobile medical device will consist of a miniaturized system worn by or embedded inside the patient, a nearby intermediate base station in range of the device’s wireless radio (which can exist in the from of a computer or smartphone), and a protected data server where information from the base station can be relayed for remote access by a caregiver or physician. The channels through which the information travels to ultimately reach the remotely located care provider open up many security vulnerabilities. Malicious hackers who can penetrate the data server could obtain and / or alter information from the device, compromising the patient’s confidentiality, privacy, and the integrity of treatment. Additionally, hackers within communication range of the device can alter its operation, posing serious risks for patient safety. In some scenarios, it has been shown that the information and the equipment needed to stage a malicious attack are readily accessible to the general public. In an effort to minimize these vulnerabilities, researchers have implemented novel protection schemes, intended specifically for wireless medical systems, and demonstrated their efficacy. Mobile medical devices are advantageous for numerous reasons, and even though they pose a set of risks that were not present with previous generations of medical equipment, the ongoing effort of researchers to secure these devices will not allow their vulnerabilities to prevent them from one day saturating the medical marketplace.
BibliographyDecuir, J. Bluetooth 4.0: Low Energy. http://chapters.comsoc.org/vancouver/BTLER3.pdf. (2010).
Hu, F. et al. Trustworthy Data Collection from Implantable Medical Devices via High-Speed Security Implementation Based on IEEE 1363. IEEE Transactions on Information Technology in Biomedicine. DOI: 10.1109/TITB.2010.2049204
Mostafalu, P. et al. Wireless Flexible Smart Bandage for Continuous Monitoring of Wound Oxygenation. IEEE Biomedical Circuits and Systems Conference. DOI: 10.1109/BioCAS.2014.6981761
Radcliffe, J. Hacking Medical Devices for Fun and Insulin: Breaking the Human SCADA System. Retrieved from https://media.blackhat.com/bh-us-11/Radcliffe/BH US 11 Radcliffe Hacking Medical Devices WP.pdf. (2011, August).
Rushanan, M. et al. Sok: Security and Privacy in Implantable Medical Devices and Body Area Networks. IEEE Symposium on Security and Privacy. DOI: 10.1109/SP.2014.40Suggested Reading
Denning, T. et al. Patients, Pacemakers, and Implantable Defibrillators: Human Values and Security for Wireless Implantable Medical Devices. Conference on Human Factors in Computing Systems – Proceedings. 2, 917-926. DOI: 10.1145/1753326.1753462
Gollakota, S. et al. They Can Hear Your Heartbeats: Non-Invasive Security for Implantable Medical Devices. Computer Communication Review. 41(4), 2-13. DOI: 10.1145/2043164.2018438
Halperin, D. et al. Security and Privacy for Implantable Medical Devices. IEEE Pervasive Computing. 7(1), 30-39. DOI: 10.1109/MPRV.2008.16See also (Links to other SHP articles)
Carp, Andrew. Wearable Technology in Industry and Consumer Culture
Chen, Cody. Flexible Circuits and Why They Matter
Levinson, Katie. Medical Equipment – Surgical Navigation
Wiegard, David. Big Data in Medical / Bioinformatics -
Katherine Malanson wrote a new post on the site Great Diseases 10 years ago

Writing in the New York Times, the actress, who had a preventative double mastectomy two years ago, says she carries a gene that gives her an elevated risk of cancer and describes the decision to undergo preventative surgery to have her ovaries and fallopian tubes removed.
Read more her full statement at NYTimes.com.
-
Trang Vuong changed their profile picture 10 years ago
-
Katherine Malanson wrote a new post on the site Great Diseases 10 years ago
 iStockphoto
iStockphotoHumiliation, fear and unpredictability all turn up the volume of pain, research shows. And meditation can turn down pain’s intensity, according to scientists who are starting to figure out why.
Read more at NPR.org.
-
Katherine Malanson wrote a new post on the site Great Diseases 10 years ago
 Matthias Kulka/Corbis
Matthias Kulka/CorbisWhen you dig into the numbers on cancer, the results are mixed. Overall, deaths are up. But survival five years after diagnosis has improved for many forms of the disease, including breast cancer.
Read more at NPR.org.
- Load More