IgE-mediated Food Allergy Response – An Overview
An allergic response to peanuts occurs as a result of abnormal activation of the immune system to externally ingested peanut protein, through a sensitization process12. When peanut protein enters the body, antigen presenting cells absorb and express the peanut allergens on their surface5. The allergens are recognized by T-lymphocyte and B-lymphocyte cells, which become antibody secreting cells. IgE antibodies are secreted into the bloodstream during allergen sensitization, which continue on to bind to the surface of mast cells via high affinity and low affinity receptors12. The IgE antibodies have specific binding capabilities for peanut proteins. Once the body is re-exposed to the threshold amount and type of allergen (in this case, peanut protein), an allergic response is initiated by the bound IgE antibodies16.
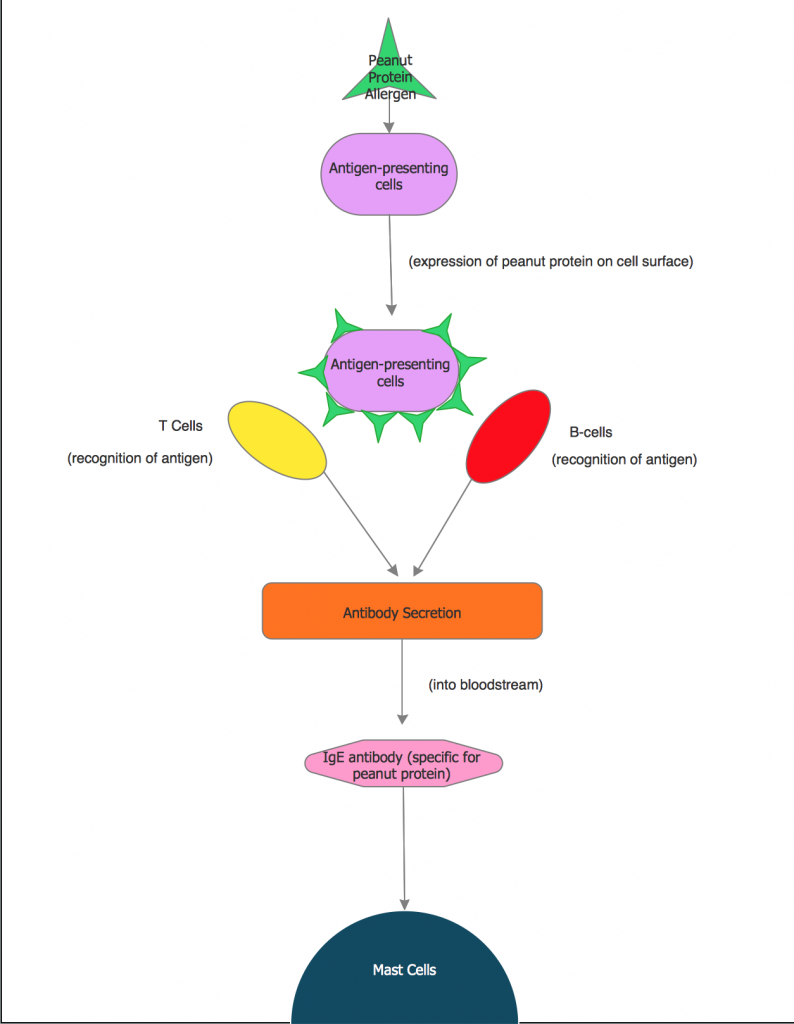
Figure 11 – An overview of IgE-mediated food sensitization.
Early Response
Mast cells reside in the mucosal and epithelial tissues of the body16. They express high-affinity receptors (FceRI) and low-affinity receptors (FceRII) on their cell surface. IgE binds to the high-affinity receptors, covering the surface of the mast cells. Once an antigen cross-links to the bound IgE, a cell-signaling cascade is initiated. Degranulation of the mast cell is activated immediately. Granules, enclosing thirty different inflammatory mediators, fuse with the plasma membrane, causing their extracellular release into the cytoplasm. These mediators include histamine, chemokines, lipid mediators, and cytokines. The molecules released trigger a wide range of symptoms in different tissues, including the smooth muscle and blood vessels. Figure 12, below, shows a schematic of this response process, with the cross-linking allergen (in green) bound to the Y-shaped immunoglobulins on the surface of the mast cell. The IgE that cross-links the antigen to the low affinity receptor enhances the allergic reaction by activating degranulation of mast cells as well as degranulation of basophils and eosinophils.
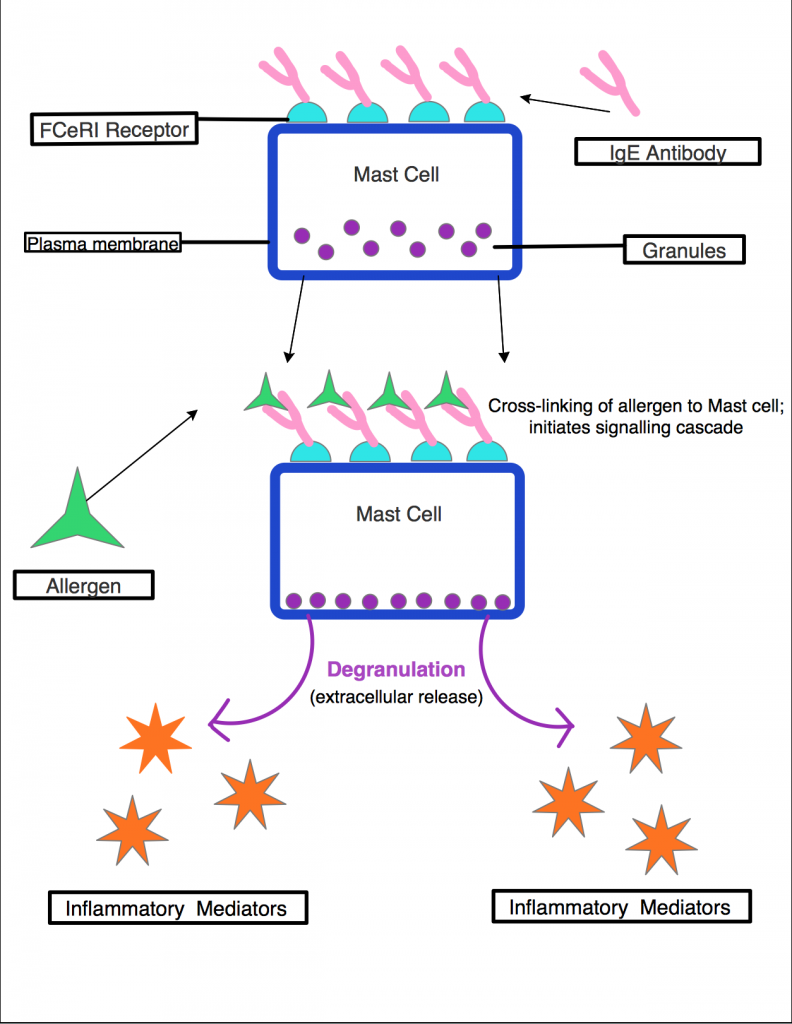
Figure 12 – Overview of the Early Response to an allergen. When IgE-specific allergen cross-links to IgE on the surface of mast cells, a signaling cascade is initiated, causing degranulation and extracellular release of chemical mediators.
Late Response
The late response can occur anywhere from 2 to 24 hours after the initial contact with an allergen16. During this phase, T helper cells (TH2) are made and recruited to tissue cells by cytokines released by mast cells during the early response. T helper cells originate in the thymus gland. Once cytokines releases from the mast cells during the early response and a specific antigen are present in an organism, T helper cells begin to divide and activate. T helper cells stimulate synthesis of IgE antibodies, acutely degranulate mast cells, and secrete cytokines such as IL-4 and Il-5, which recruit basophils and eosinophils respectively to the site of inflammation. These molecules cause prolonged tissue damage as well as a sustained inflammatory responses (despite a lack of allergen present). The late response has a less severe effect on the body than the immediate early phase response, and in some cases does not occur at all. When it does occur, it causes the same symptoms as the early response. It is most often seen in cases of allergic asthma and allergic rhinitis, two examples of conditions involving chronic inflammatory responses to allergen exposure.16
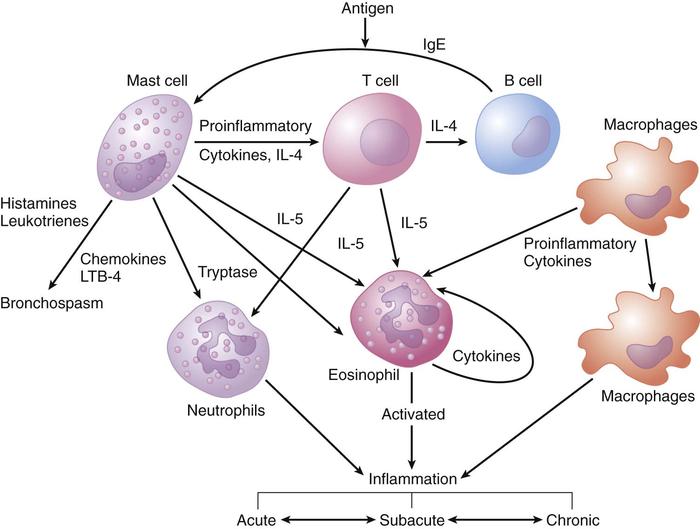
Figure 13: An overview of the early (acute), late (subacute), and chronic responses to allergens.17
Role of Eosinophils and Basophils
As part of the late-response to the cross-linking of a food allergen to IgE, chemical mediators and T helper cells (TH2) activate eosinophils and basophils. Basophils share a similar structure to mast cells, and are differentiated in bone marrow. They express FceRI on their cell surface, and when an allergen (such as peanut protein) cross-links to the receptor, granule exocytosis and the release of chemical mediators is initiated16. Basophils primarily release IL-3, Il-4, and histamine into inflamed tissues, including the skin and the airway, during allergic reactions16. Eosinophils are granulocytes which also release chemical mediators into the bloodstream, although not through FCeRI cross-linking16. They contain many other forms of receptors, including those for cytokines, leukotrienes, and platelet activating factor. Trafficking of eosinophils to sites of allergic inflammation is promoted by the release of Il-3 and Il-4 by basophils. Once activated through cell-surface reception, the eosinophils release inflammatory cytokines as well as lipid mediators such as platelet activating factor (PAF) and leukotrienes16. Both eosinophils and basophils are responsible for causing inflammation and tissue damage in response to an allergen.
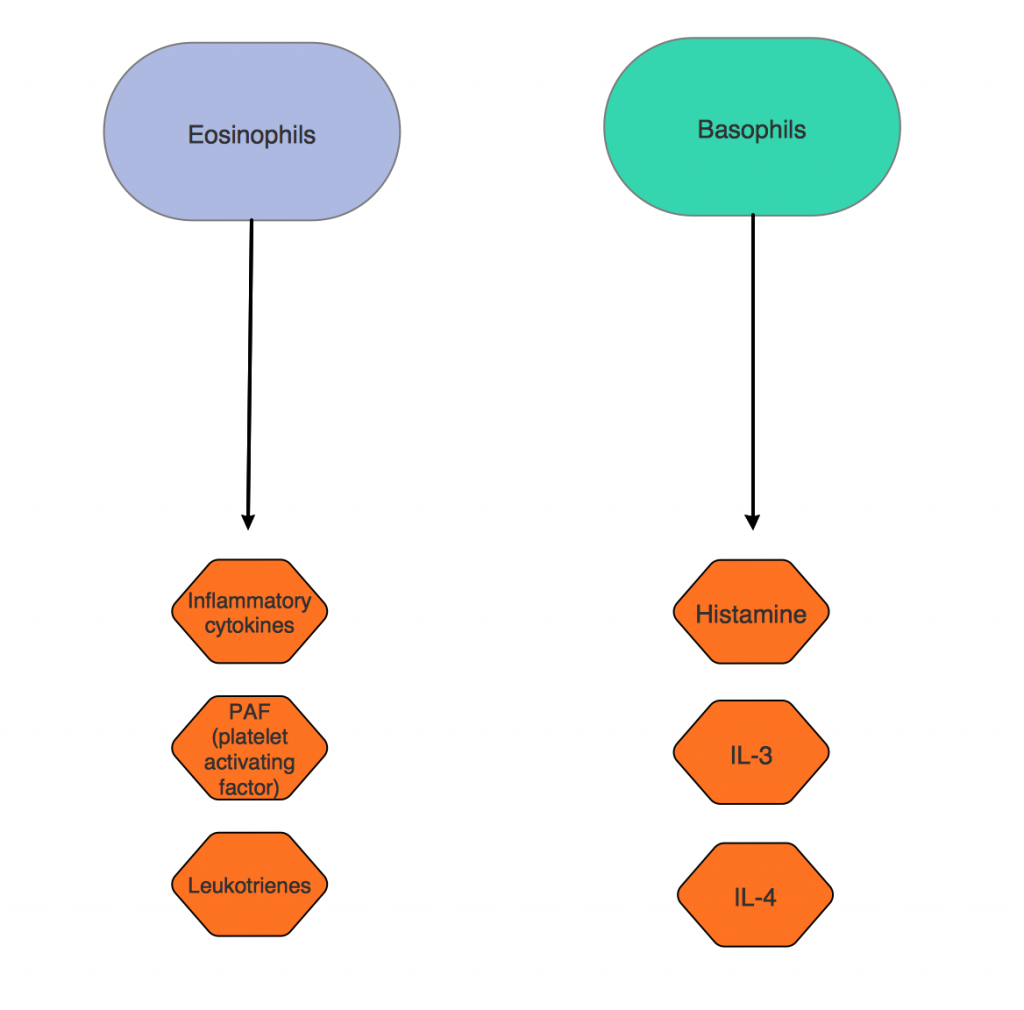
Figure 14 – The role of eosinophils and basophils in an IgE-mediated allergic response. Eosinophils are responsible for the extracellular release of inflammatory cytokines, toxic granular proteins, and lipid mediators such as platelet activating factor and leukotrienes at the sites of allergic inflammation. Basophils release the majority of histamine, Il-3, and IL-4 into the bloodstream during an allergic response.
Effect of Chemical Mediators:
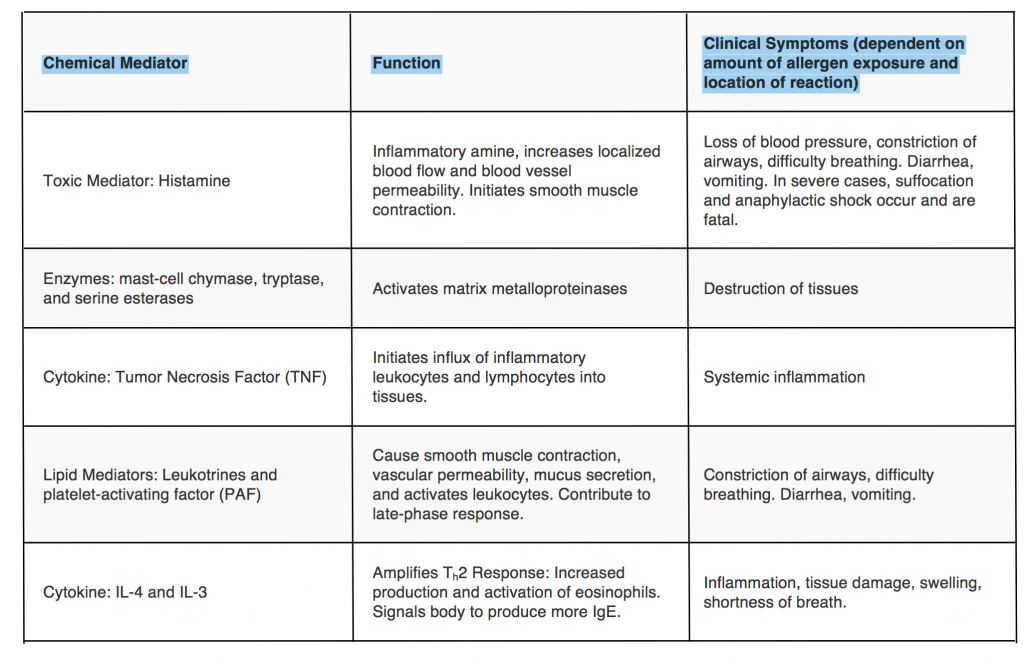
Table 1 – Chemical Mediator Chart. The individual effects of chemical mediators released during the IgE-mediated response are explored in greater detail5.
In the first two pages the figure numbering is restarted each time, but here it appears to be a continuation of figure numbering on the previous page. I’d suggest picking one numbering method and keeping it consistent throughout the website.
This page has great explanations and figures, but I wonder if including a quick figure or paragraph comparing early and late responses would be useful. After reading through the first time, it was hard to determine the differences in symptoms/physiological results of early vs late response as they both seemed to just cause inflammation and tissue damage. I definitely do like the pathway figures however so don’t remove those if you do consider this suggestion.
The next time I read a blog, Hopefully it doesn’t disappoint me as much as this one. I mean, I know it was my choice to read through, however I actually believed you would probably have something useful to talk about. All I hear is a bunch of complaining about something you could possibly fix if you weren’t too busy searching for attention.
Hello tufts.edu owner, Your posts are always well-referenced and credible.
Zajrzyj na naszą stronę, jeśli chcesz dowiedzieć się więcej na temat upadłości konsumenckiej.
The articles you write help me a lot and I like the topic