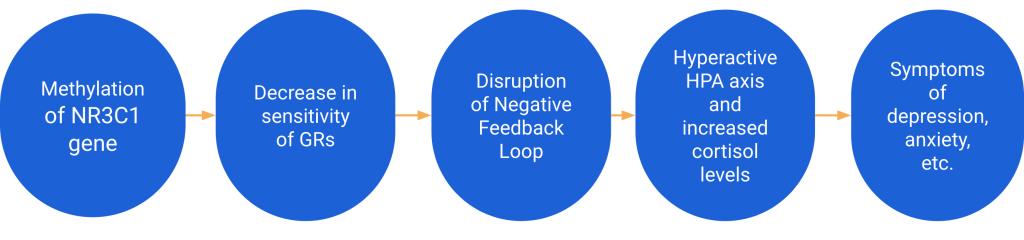
In studies of Vietnam War veterans, Holocaust survivors, and their offspring, altered methylation patterns at the NR3C1 gene were found to be associated with symptoms of PTSD and mental illness (2,3). The methylation of this gene in the paternal germline (F0 generation) was also found to be strongly associated with mental illness in the offspring (F1 generation) (2). Additionally, the NR3C1 gene was found to be resistant to reprogramming in zygote formation, meaning that the methylation patterns of the NR3C1 in parental DNA can be passed on to their children (18). To learn more about resistance to reprogramming visit our page: Genetic Reprogramming.
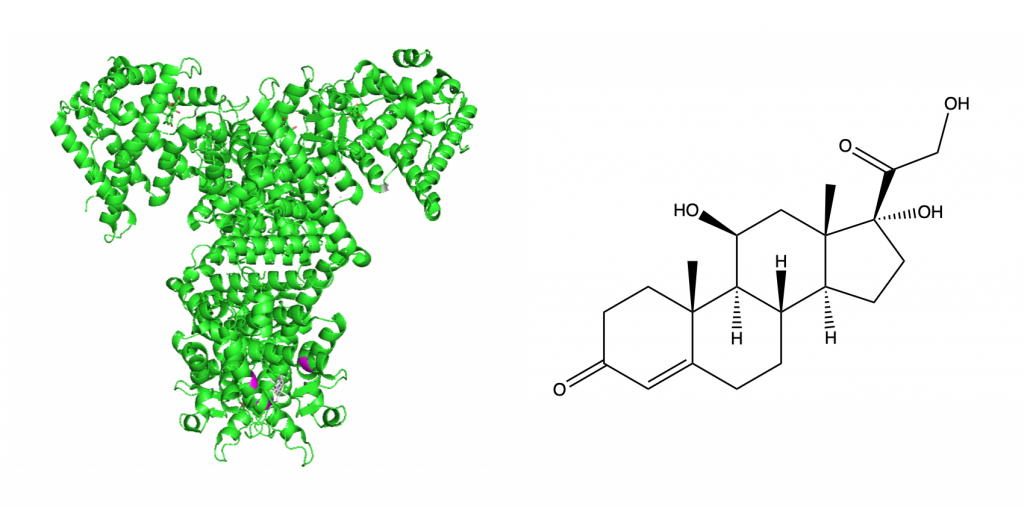
NR3C1 is the gene that codes for glucocorticoid receptors. Glucocorticoid receptors (GRs) are important proteins for controlling the body’s stress response. Glucocorticoids (GCs) are steroid hormones that the adrenal gland secretes. GRs are present in the cytoplasm of almost all cells and become activated when bound to cortisol — a glucocorticoid and the main stress hormone in humans. Once activated GRs act as transcription factors (21). Because of their ubiquity, GCs and GRs can have many different effects on the body in areas including metabolism, immune response, and stress response (23). This page focuses on the relationship between GRs, stress response, and their connection to mental illness.
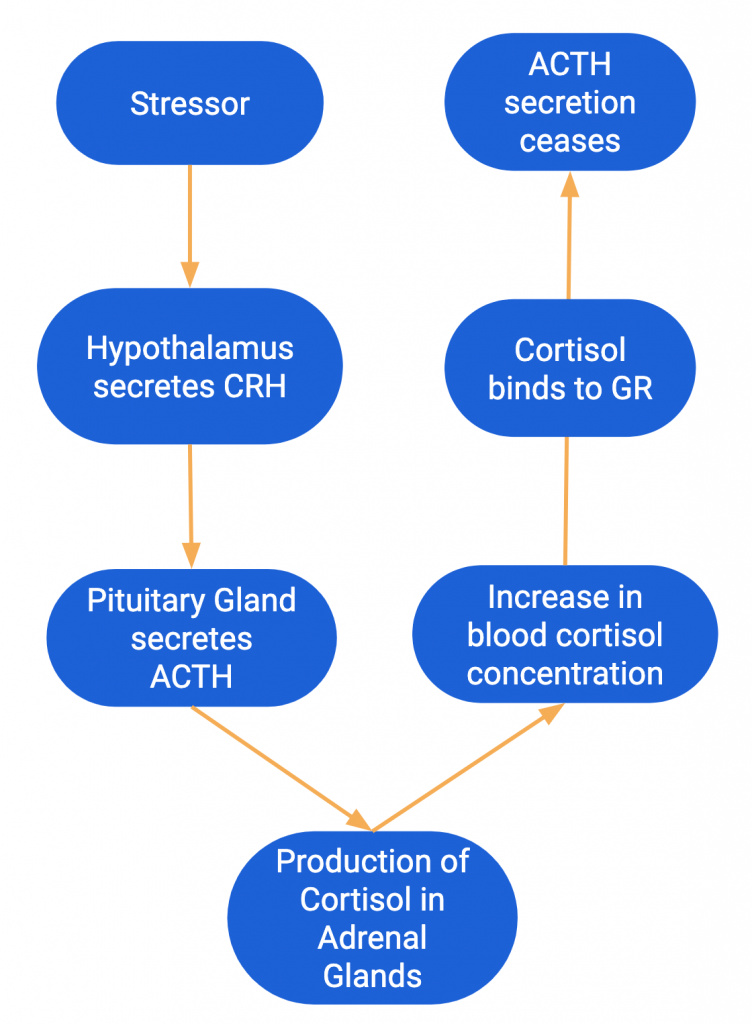
Glucocorticoid receptors function as part of the Hypothalamic-Pituitary-Adrenal (HPA) axis. The HPA axis regulates the release of corticotropin releasing hormone (CRH) and adrenocorticotropic hormone (ACTH), and cortisol. When exposed to a stressor the hypothalamus secretes CRH and then the pituitary gland releases ACTH. The release of ACTH signals the adrenal glands to produce cortisol. As the concentration of cortisol in the blood increases, cortisol binds to GRs (4, 5).
GRs help regulate the activity of the HPA axis through a negative feedback loop (4). Cortisol binding to GRs is critical for this feedback. Once cortisol binds to GRs, the HPA axis stops producing CRH and ACTH, which then causes cortisol production to cease. This negative feedback inhibition allows for the body to maintain relatively constant levels of cortisol in the blood (5).
The offspring of male Holocaust survivors with PTSD were found to have high methylation at the GR-1f promoter (3). This hypermethylation changes the efficacy of GR function in the HPA axis. Methylation of the GR gene represses transcription, so fewer GRs are expressed in cells. The decrease in gene expression leads to a decrease in glucocorticoid sensitivity (3). A decrease in sensitivity means that cortisol is less likely to bind to GRs. When there is less binding of cortisol to GRs, the negative feedback inhibition loop is disrupted. The disruption causes higher cortisol levels as well as hyperactivity in the HPA axis (i.e. the HPA axis continues to secrete CRH and ACTH and produce cortisol). Hyperactivity and dysregulation of the HPA axis are common in mental illnesses like depression, anxiety, and PTSD (4).

I think it would be helpful to mention where the GR are in the body, and maybe also where cortisol is produced, just to get an idea of where this is taking place in the body.
One small thing i would note is that in your figure 9, the process you describe starts with “stress” I think that stress is an emotional and biological result of this process, but ACTH release is triggered by a “stressor” some stimulus that causes the stress response in the body, but the stress response is not triggered by stress itself.
Beyond these two small things, I think this page is really well done. You have condensed a complex endocrinological process into a very logical and easy to understand process and tied the biochemical process to the physical expression of mental illness in a very understandable way.
I agree completely with the points you made. I’ve make the changes you suggested.
I have a question about where exactly cortisol is produced. Is the cortisol produced within the brain? Or does the ACTH instead go somewhere else within the body to signal the production of cortisol. Also, how exactly does the cortisol molecule pass through the blood brain barrier? Is it able just to slip in-between? This page mentions how the blood levels of the cortisol can directly affect the GRs located within the HPA axis, so can cortisol just pass through the blood brain barrier without being stopped?
I’ve added some specific of which glands produce which hormones in the HPA axis pathway discussed. I hope this helps clarify when in the body it’s all happening. I also added the structure of cortisol and a note in the figure description about how it can pass through the blood brain barrier.
I agree with the above comments, and also suggest that a short description be added about glucocorticoids–namely, what they are and how they function on a chemical level–and more differentiation regarding in which organ systems these processes are involved.
I’ve added a sentence to clarify what glucocorticoids are in general. I don’t want to get too deep into all of the processes they are involved in because there are a lot especially because they are present everywhere in your body, but I added a sentence acknowledging their versatility and ubiquity to address this concern because I think it is a good point.
This is a very full and comprehensive page; whenever I found myself with a lingering question at the end of a paragraph it was often answered by the next one which is a sign of a well-though out page.
Just make sure to check through your figure (some formatting broke words apart, keep consistent capitalization schemes, etc).
Done!