During the novel coronavirus disease 19 (COVID-19) pandemic, countries worldwide have developed temporary medical facilities to provide sufficient testing and care to infected persons [1–5]. An extension of combat support hospitals and field hospitals, these facilities commonly provide emergency medical services during military deployment [6,7]. However, in recent years many countries have begun deploying these temporary hospitals to provide emergency services and supplies during natural disasters and humanitarian emergencies [8,9].
Throughout the COVID-19 pandemic, these facilities have faced growing volumes of infected persons and have lacked sufficient personnel, medical supplies, medical equipment, and bed capacity to effectively house and treat patients. Safety concerns for medical personnel have also inhibited the delivery of care by reducing patient interaction, wearing personal protective equipment, and performing medical assessments while practicing social distancing [10]. These challenges especially inhibit medical staff providing nutrition services where patient interaction is consistently needed to monitor nutrition status and deliver therapeutic meals multiple times per day during a patient’s hospital stay [10]. Furthermore, these nutrition operations require careful coordination and management of food contracts and supplies, which must be consistently monitored to ensure accessibility of patient meals and continuity of food safety, respectively.
In review of the Accreditation Council for Education in Nutrition and Dietetics’ Accreditation Standards for Nutrition and Dietetics Internship Programs, under ‘Domain 4. Practice Management and Use of Resources: Strategic application of principles of management and systems in the provision of services to individuals and organizations,’ training competencies lack mention of food contracts or the development of skills necessary to implement and sustain food contracts, which are becoming vital skills in response to COVID-19 [11]. Furthermore, these resources fail to provide sufficient training on managing food contracts, staffing nutrition personnel, recording patient nutrition status, or administering nutrition assessments in emergency or disaster relief efforts. Without these resources, nutrition personnel cannot sufficiently prepare for field hospital deployments and must modify existing nutrition assessments that are not designed for resource sparse settings. These challenges necessitate a central technical report created to inform nutrition protocols and assessments in emergency response settings for clinical nutritionists, dietitians, and personnel.
To promote preparedness plans for nutrition response in future humanitarian crises, we develop this Nutrition Response Toolkit for Humanitarian Crises to provide a standardize nutrition-focused protocols for implementation in future field hospital deployments or humanitarian emergency facilities. For each proposed tool, we explain that tool’s purpose and utilization, provide an example of how to implement this tool in the field, and provide a fillable form for use in crisis settings.
References
- Sisak, M. Many Field Hospitals Went Largely Unused, Will Be Shut Down. Military Times 2020.
- Mash, R.; Presence-Vollenhoven, M.; Adeniji, A.; Christoffels, R.; Doubell, K.; Eksteen, L.; Henrikse, A.; Hutton, L.; Jenkins, L.; Kapp, P.; et al. Evaluation of Patient Characteristics, Management and Outcomes for COVID-19 at District Hospitals in the Western Cape, South Africa: Descriptive Observational Study. BMJ Open 2021, 11, e047016–e047016, doi:10.1136/bmjopen-2020-047016.
- Francke, R.-L. Covid-19 Field Hospital Opens in Mitchells Plain. IOL News 2021.
- Canadian Press Ontario Says a COVID-19 Field Hospital Is Expected to Take Patients This Month. CTV News 2021.
- BBC Wales Covid-19: Are Field Hospitals Operating in Wales? BBC News 2020.
- Lewis, M.M.; Bower, A.; Cuyler, M.T.; Eden, R.; Harper, R.E.; Gonzalez Morganti, K.; Resnick, A.C.; Steiner, E.D.; Valdez, R.S. New Equipping Strategies for Combat Support Hospitals. RAND Health Quarterly 2012, 2, 2.
- LaBrecque, M.F.; Honsberger, M.A. Army Field Hospitals and Expeditionary Hospitalization; Army Sustainment Professional Bulletin; United States Army, 2018.
- Davis, L.E.; Rough, J.; Cecchine, G.; Schaefer, A.G.; Rohn, L.L. Hurricane Katrina: Lessons for Army Planning and Operations; RAND Corporation, 2007; p. 106.
- Larson, E.V.; Boling, B.; Eaton, D.; Genc, S.; Kravitz, D.; Leuschner, K.J.; Lewis, A.; Liggett, J.; Polley, L. U.S. Army North in the Hurricane Maria Response; RAND Corporation, 2020; p. 236.
- Sanchez, E.; Gelfand, A.R.; Perkins, M.D.; Tarnas, M.C.; Simpson, R.B.; McGee, J.A.; Naumova, E.N. Providing Food and Nutrition Services during the COVID-19 Surge at the Javits New York Medical Station. In Review 2021.
- Accreditation Council for Education in Nutrition and Dietetics ACEND Accreditation Standards for Nutrition and Dietetics Internship Programs (DI); Academy of Nutrition and Dietetics, 2018.
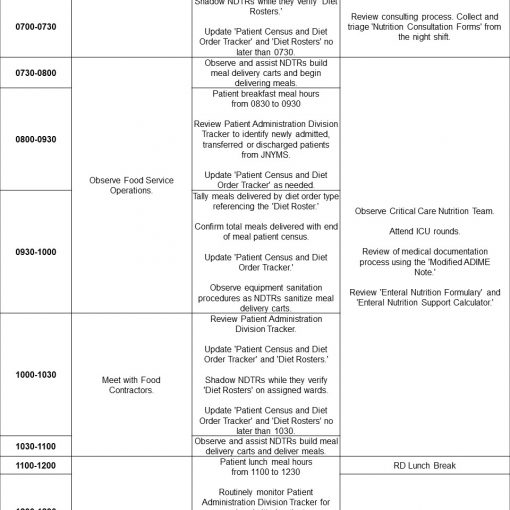
This toolkit includes guidance for every step of staffing a field hospital, establishing nutrition-focused medical records, and monitoring patient nutrition status. Using this order of operations, we have designed the toolkit to have the following structure:
- Establishing a Field Hospital Nutrition Operations Team
- Staffing model for emergency settings
- Two-day staffer training program
- Monitoring Inpatient Nutrition Status
- Screener for inpatient nutrition status
- Modified ADIME note
- Tracker for patient census and diet orders
- Diet roster
- Receiving Nutrition Concerns from Field Hospital Staff
- Nutrition consultation form
- Diet order change and supplement request form
- Food temperature log
- Calculating Patient Nutrition Support Needs
- Guide for enteral formulary
- Enteral nutrition recommendation calculator
As the COVID-19 pandemic continues, we call upon the broader research and practice community, including the Academy of Nutrition and Dietetics, to develop guidelines for nutrition services in medical facilities. These guidelines must target training competencies for RDs, NDTRs, and other nutrition-related personnel providing medical care in field hospitals or emergency facilities during humanitarian crises. While the Nutrition Response Toolkit for Humanitarian Crises provides a foundation for such services, this toolkit must be expanded to enhance the scalability and generalizability of these tools for future emergency response efforts. This can only be done by collaborating with other medical and nutrition service professionals, who together can document shared and new experiences that warrant new tools for field response-related challenges. We welcome this future collaboration, and hope that these low-cost, easily-adaptable nutrition services and assessments tools can be aid nutrition personnel in future field hospital deployments and humanitarian emergencies.
The first draft of this toolkit was prepared by Emily Sanchez, MS, RD, CNSC of the Tufts University Friedman School of Nutrition Science and Policy and Army Medical Department Student Detachment, U.S. Army Medical Center of Excellence, Amy R. Gelfand, MS, RD, CNSC of the Bureau of Supplemental Food Programs, New York State Department of Health, Michael D. Perkins, MS, RDN of the Bureau of Supplemental Food Programs, New York State Department of Health, Maia C. Tarnas of the Community Research Initiative of New England, Ryan B. Simpson, MS of the Tufts University Friedman School of Nutrition Science and Policy, Jarrod A. McGee, FACHE, MHA, MBA of Army-Baylor University and the United States Army 1st Medical Brigade, William Beaumont Army Medical Center, and Dr. Elena N. Naumova of the Tufts University Friedman School of Nutrition Science and Policy.
The authors thank the Nutrition Operations Team and multi-agency collaborators at the Javits New York Medical Station, to include the New York State Department of Health, for their commitment to data collection in support of improving disaster response efforts for nutrition personnel.
Sanchez, E.; Gelfand, A.R.; Perkins, M.D.; Tarnas, M.C.; Simpson, R.B.; McGee, J.A.; Naumova, E.N. Nutrition Response Toolkit for Humanitarian Crises; Tufts Initiative for the Forecasting and Modeling of Infectious Diseases: Gerald J. and Dorothy R. Friedman School of Nutrition Science and Policy, Tufts University, 2021; https://sites.tufts.edu/naumovalabs/crisisnutritiontoolkit/.