When planning for a potential use of a field hospital, one must remember that field hospitals are modular medical treatment facilities generally designed to provide medical capabilities in a deployed setting [1]. Within the field hospital, it is the responsibility of nutrition care operations, which primarily consists of Registered Dietitians (RDs) and Nutrition Dietetics Technicians, Registered (NDTR), to provide services that include meal preparation and service to patients, medial nutrition therapy, dietetic planning and patient education [2]. Hospital food service and clinical nutrition operations are essential to ensure patients receive sufficient nutrition to prevent complications associated with malnutrition, while complying with the appropriate diet orders given their medical diagnosis [2]. Yet in the wake of a humanitarian crisis, no single staffing model exits for nutrition response in field hospitals [3]. With that in mind, we provide examples of a staffing model and personnel training program that can assist in establishing nutrition services within an emergency field hospital or medical facility.
References
- LaBrecque, M.F.; Honsberger, M.A. Army Field Hospitals and Expeditionary Hospitalization; Army Sustainment Professional Bulletin; United States Army, 2018
- United States Army Theater Hospitalization; Department of the Army: Headquarters, 2020.
- Joint Commission Surge Hospitals: Providing Safe Care in Emergencies; Joint Commission on Accreditation of Healthcare Organizations, 2006.
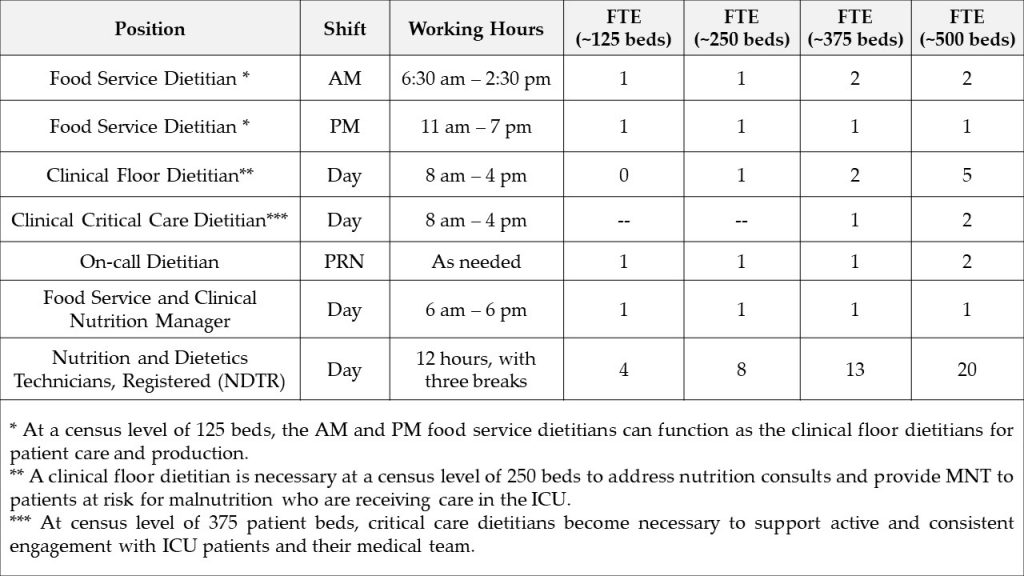
Purpose: The Field Hospital Staffing Model is designed to identify staffing needs for nutrition services in a field hospital or emergency facility setting with 125-500 patient beds. This model accommodates for extended time needed to complete patient assessments due to the absence of an EMR, donning and doffing full PPE, locating patients amid transfers, coordinating care with medical and nutritional personnel, documenting MNT recommendations, and balancing the completion of clinical and food service roles.
Utilization: This tool should be referenced during the planning phase of a field hospital mobilization. This model assumes that: i) nutrition operations are functional during a 12-hour period, e.g., 6:30 am – 6:30 pm, seven days per week; ii) the field hospital serves a patient census ranging from 125-500 patients per day; and iii) RDs have limited capacity (3-4 patients daily) to provide clinical care.
Example of a Field Hospital Staffing Model used at the Javits New York Medical Station from 28 April through 01 May of 2020:
Food Service Dietitians provide nutrition care to patients to prevent malnutrition and optimize recovery. Primary responsibilities include:
- AM Food Service Dietitian:
- Assessing menus and diet orders to ensure food items are appropriate
- Delivering meals safely at breakfast and lunch
- Confirming patient census, diet orders and creating diet production sheets
- Administering production sheets to NDTRs
- Supervising NDTRs preparing meal delivery carts
- Overseeing diet order and food allergy questions/concerns
- Answering questions regarding diet orders and assisting with appropriate food substitutions
- Implementing and maintaining adherence to food safety and equipment sanitation protocols
- Ensuring food waste is properly discarded after meal delivery service
- Checking floor nourishment par levels and confirming delivery of more stock items
- At census levels of <125 patients: assessing patients identified at risk for malnutrition high risk patients and providing nutrition consultations
- At census levels of <250 patients: assisting clinical floor dietitians as needed
- PM Food Service Dietitian:
- Assessing menus and diet orders to ensure food items are appropriate
- Delivering meals safely at dinner
- Confirming patient census, diet orders and updating diet production sheets for dinner
- Administering production sheets to NDTRs
- Supervising NDTRs preparing meal delivery carts
- Overseeing diet order and food allergy questions/concerns
- Answering questions regarding diet orders and assisting with appropriate food substitutions
- Implementing and maintaining adherence to food safety and equipment sanitation protocols
- Ensuring food waste is properly discarded after meal delivery service
- At census levels of <125 patients: assessing patients identified at risk for malnutrition high risk patients and providing nutrition consultations
- At census levels of <250 patients: assisting clinical floor dietitians as needed
Clinical Dietitians provide nutrition care to patients to prevent malnutrition and optimize recovery. Primary responsibilities include:
- Clinical Floor Dietitian:
- Providing nutrition care and management of patients in a general medicine setting
- Interpreting physician diet orders and modifying diet according to diet patterns and patient preferences
- Conducting clinical nutrition assessments on patients identified at risk for malnutrition via the Nutrition Screening Form (see Section 3. Monitoring Inpatient Nutrition Status) or the Nutrition Consult Form (see Section 4. Receiving Nutrition Concerns from Field Hospital Staff)
- Providing MNT recommendations (i.e., chronic disease management and strategies to improve food intake during hospital admission)
- Making appropriate recommendations for nutrition care including but not limited to:
- Oral supplements
- Nutrition supplements
- Food-drug interactions
- Communicating nutrition recommendations through appropriate medical documentation using the ADIME format
- Completing calorie counts
- Attending medical rounds and patient care plan meetings
- Coordinating care with patient’s primary care manager (PCM) and case management
- Communicating nutrition recommendations for assigned patients to food service staff
- Maintaining open communication between the hospital staff and Nutrition Operations
- Clinical Critical Care Dietitian:
- Conducting nutrition assessment on patients in the ICU
- Interpreting physician diet orders and modifying diet according to diet patterns and patient preferences
- Conducting clinical nutrition assessments on patients identified at risk for malnutrition via the Nutrition Screening Form (see Section 3. Monitoring Inpatient Nutrition Status) or the Nutrition Consult Form (see Section 4. Receiving Nutrition Concerns from Field Hospital Staff)
- Providing medical nutrition therapy recommendations including but not limited to:
- Enteral nutrition support
- Parenteral nutrition support
- Oral supplements
- Nutrition supplements
- Food-drug interactions
- Communicating nutrition recommendations through appropriate medical documentation using the ADIME format (see Section 3. Monitoring Inpatient Nutrition Status)
- Attending medical rounds and patient care plan meetings with ICU team
- Coordinating care with patient’s PCM and case management
- Performing patient handoff to floor dietitian if patient transferred out of the ICU
On-Call Dietitians serve as backup dietitians in the event of an illness or emergency. On-call dietitians share the responsibilities of food service and clinical dietitians.
Food Service and Clinical Nutrition Manager provides leadership, oversight and direction to both the food service and clinical staff. Primary responsibilities include:
-
- Attending field hospital leadership and operations meetings and monitoring staffing needs
- Assessing menus and diet orders to ensure food items are appropriate
- Leading the administration and coordination of the food service contract with the onsite vendor
- Working with vendor, clinical staff, and field hospital leadership to assess and coordinate procurement of patient meals
- Coordinating with vendors and production dietitians to assess appropriateness of food items for each diet order and obtaining allergen information for each food item
- Leading communications with the clinical dietitians and assessing ongoing staffing needs
- Ensuring adherence to food safety and clinical nutrition policies
Nutrition and Dietetics Technicians, Registered (NDTR) provide nutrition care to patients to prevent malnutrition and optimize recovery. Primary responsibilities include:
-
- Performing malnutrition screening using the Nutrition Screening Form and referring patient to a clinical dietitian as needed
- Collecting data on the patient’s dietary preferences, food allergies and/or intolerances
- Verifying diet ward rosters before each meal delivery
- Communicating roster updates to food service dietitians
- Preparing patient meal delivery carts
- Delivering patient meals
- Following food safety and equipment sanitation protocols
- Supporting maintenance of Patient Census and Diet Order Tracker (see Section 3. Monitoring Inpatient Nutrition Status)
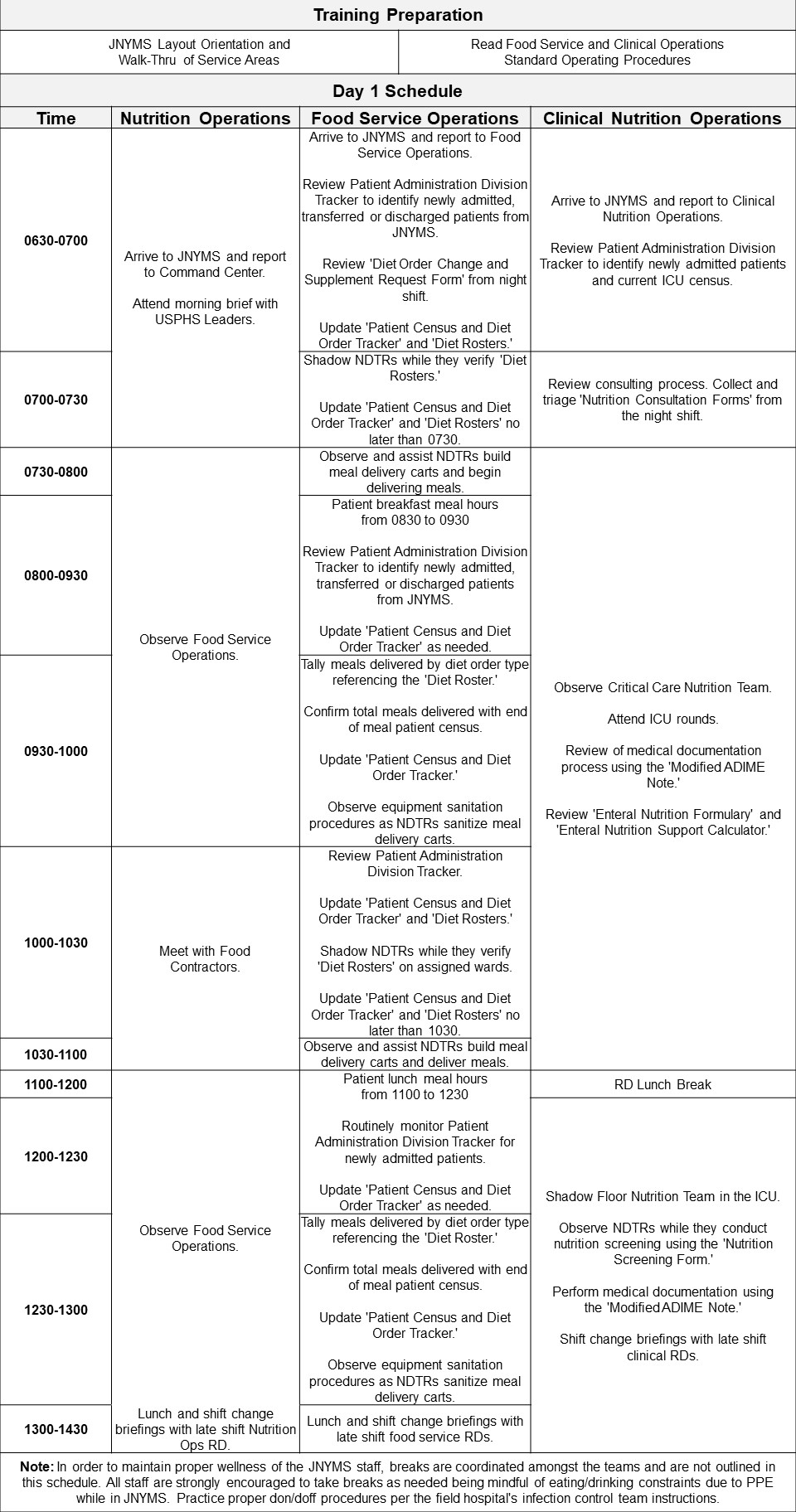
Purpose: The Training Program Syllabus is designed to orient new RDs and offer appropriate training on food service management, clinical nutrition, and nutrition support operations. These trainings should explain the organization of the field hospital, operational mandate for nutrition services, and coordinated protocol for simultaneously managing food services and performing clinical nutrition evaluations.
Utilization: This tool should be referenced during the planning phase of field hospital mobilizations and when onboarding new RDs. This comprehensive two-day training resource helps orient civilian RDs and offer appropriate training on food service management, clinical nutrition, and nutrition support operations for RDs who lack sufficient clinical experience.
Example of Training Program Syllabus used at the Javits New York Medical Station from 28 April through 01 May of 2020: