GIP-Mediated Communication of Pancreatic α-cells and β-cells Leads to Increased Insulin Secretion
Overview:
The paper “GIP mediates the incretin effect and glucose tolerance by dual actions on α cells and β cells” [19] focuses on the role of the glucose-dependent insulinotropic polypeptide (GIP) in regulating insulin and glucagon secretion – both of which are crucial for glucose homeostasis. The role of GIP, a hormone communicating nutrient intake from the gut to pancreatic islets, is discussed to have dual actions on both pancreatic α cells and β cells. In α cells, GIP potentiates amino acid–stimulated glucagon secretion, while in β cells, it enhances insulin secretion. Although these hormones seem to have opposite roles, the duality of GIP is significant in maintaining postprandial (after lunch or dinner) homeostasis.
Results & Analysis:
The research demonstrates that GIP’s action in α cells is necessary for coordinating optimal levels of both glucagon and insulin to maintain glucose levels post-meal. It also shows that GIP-stimulated glucagon secretion can enhance insulin secretion beyond direct GIP receptor activity in β cells alone, pointing to an intricate interplay in glucose regulation. The mechanism of communciation between α and β cells is described with more detail in the Glucagon-Mediated Insulin Secretion After Fasting section.
Significance & Connection to Type II Diabetes:
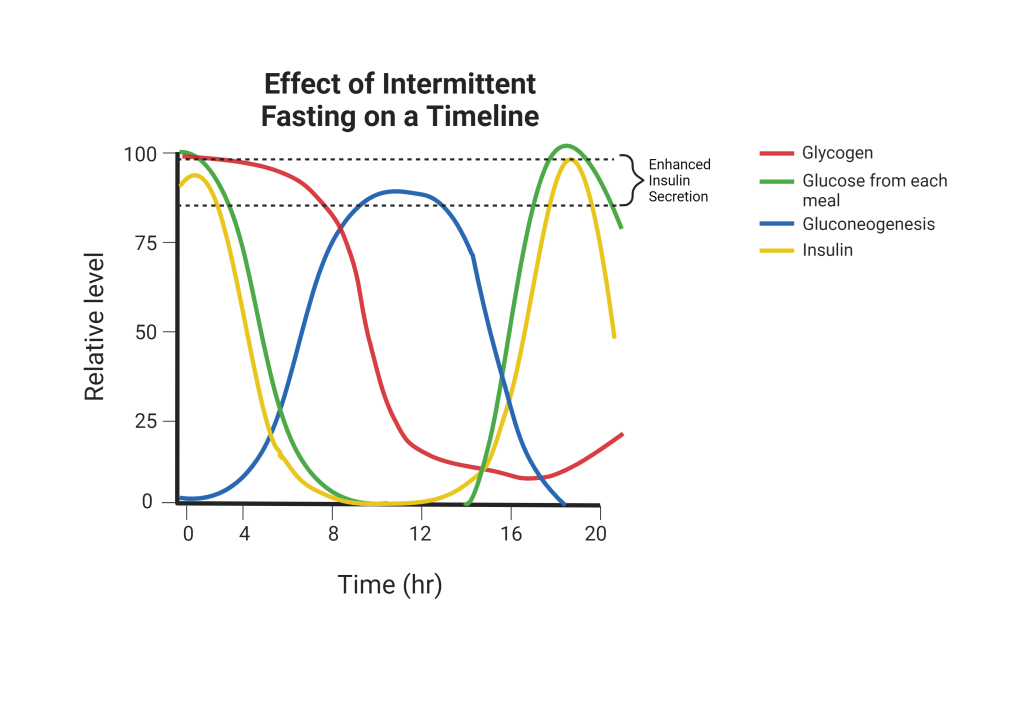
The findings of this study can be applied to intermittent fasting and its impact on individuals with type II diabetes who do not secrete enough insulin. By altering the pattern of nutrient intake, intermittent fasting depletes cellular glycogen supplies after each meal and initiates gluconeogenesis by converting amino acids into free glucose. During gluconeogenesis, the amino acid alanine stimulates glucagon secretion in α cells and further enhances glucagon-stimulated insulin secretion in β cells. An intermittent fasting regimen modulates the secretion and action of GIP, thereby affecting insulin and glucagon levels. The enhanced insulin secretion caused by this series of reactions happens 12-16 hours after a meal, which is the time that intermittent fasting ends and the next meal comes in. The temporal pattern of various metabolic processes involving glucose is demonstrated below in Figure 1.
Type II diabetics are resistant to insulin or do not produce enough. Therefore, the fasted state increases insulin secretion through raising free alanine levels that trigger the aforementioned α-β cell communication. This paper inspired us to discover new and interesting ways in which intermittent fasting impacts type II diabetics on a molecular level.
December 4, 2023 at 5:44 pm
I thought this page was great. I would maybe include some information in figure 1 and the final paragraph concerning the impact of GIP specifically. I feel that with your awesome information in the previous paragraph, the final couple sentences at the bottom are not entirely necessary, at least in the page position that they are in now. Good job!
December 5, 2023 at 2:17 am
Awesome job in breaking down this article! I thought the analysis of this paper was done concisely and to the point. However, I still have a bit of confusion regarding how the alanine/GIP-stimulated release of Glucagon isn’t harmful for patients with Type II diabetes. While the page outlines how Glucagon can boost insulin secretion beyond direct GIP receptor activity in β cells, I believe this concept requires more clarification on how the release of insulin effectively lowers blood sugar levels despite the presence of Glucagon. Additionally, I’m uncertain about the source of information used in creating Figure 2. Although it’s a visually effective diagram showcasing the effects of intermittent fasting, the lack of proper citation raises concerns about its credibility. Was this taken from the paper or was it from our Biochemistry lectures?
December 5, 2023 at 8:45 pm
The analysis of the paper was beautifully summarized, and I really enjoyed seeing a rendition of the diagram that we saw in Lecture 12, with the addition of an insulin dataset as well. Your explanation of how each curve was affected over time during intermittent fasting in the caption made interpreting the graph incredibly easy to follow, even if someone didn’t know anything about glycogen breakdown/gluconeogenesis. Furthermore, I like how you explained complicated nomenclature (i.e. “postprandial”) and utilized the graph to demonstrate the intricacies of the fluctuations caused by regulation depending on what is needed at the time (i.e. more insulin from beta cells or more glucagon from alpha cells). Perhaps this graph could be modified to additionally show peak alpha-cell or beta-cell activity, to further understand the interconnection at play. Awesome work!
December 8, 2023 at 7:06 pm
Great summary in the results and analysis section. I am not totally sure what this article has to do with mitigating the effects of type II diabetes if type II diabetics won’t respond to insulin anyway. Is this to say that intermittent fasting mimics the normal time your body will run out of glycogen, making the effects of type II diabetes less extreme? Thus, I think more elaboration on the significance and connection section would be very beneficial. I also really liked the figure, which made understanding the significance and connection section easier.
December 10, 2023 at 5:25 pm
I really liked clear result and analysis section followed by their significance to type II diabetes. It is not entirely clear how the increased insulin secretion ultimately alleviates the symptoms of type II diabetes. Reading the significance section, I think it is implied that the elevated insulin level improves the individuals ability to respond. I still think the final paragraph would benefit from further explanation on the implication for individuals with resistance to insulin and individuals who do not secrete sufficient amount of insulin.