3. Glucagon-Mediated Insulin Secretion After Fasting
Type II diabetes is characterized by a state of insulin resistance or insufficient secretion of insulin by pancreatic beta-cells. Improvement of insulin sensitivity for type II individuals is described in the previous pathways, 1. Circadian Rhythm and Glucagon Regulation of Cyclic AMP Element-Binding Protein (CREB), 2. Ketone Body Reduction of Oxidative Stress. However, this pathway provides insight into how intermittent fasting can improve insulin secretion in these cells, which is another characteristic of type II diabetes.
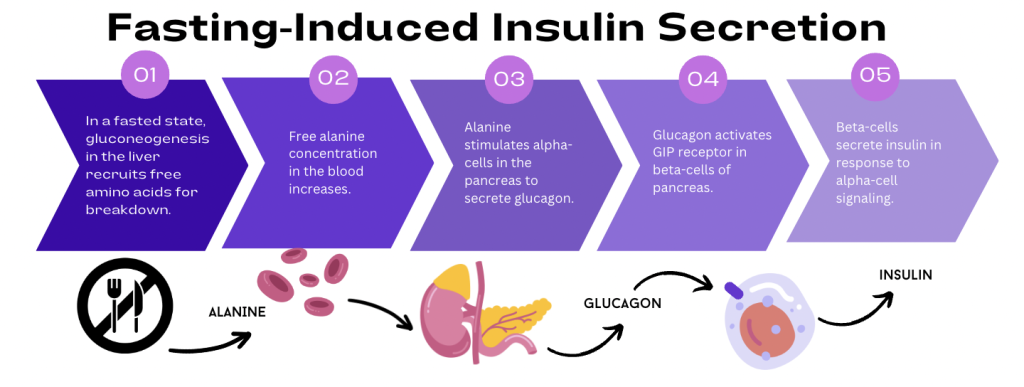
During a period of prolonged fasting, the liver will begin the process of gluconeogenesis. Blood concentrations of alanine and other amino acids have been found to increase after periods of fasting [18]. In simple terms, the liver uses the carbon skeletons of amino acids and other precursors and converts them into new glucose molecules to be released into the bloodstream.
Unlike other amino acids, alanine stimulates specific cells in the pancreas that are responsible for the release of various hormones: alpha (α) cells are responsible for glucagon secretion, while beta (β) cells are responsible for insulin secretion. These hormones have opposing effects on glucose metabolism, so their dual regulation is essential for homeostasis.
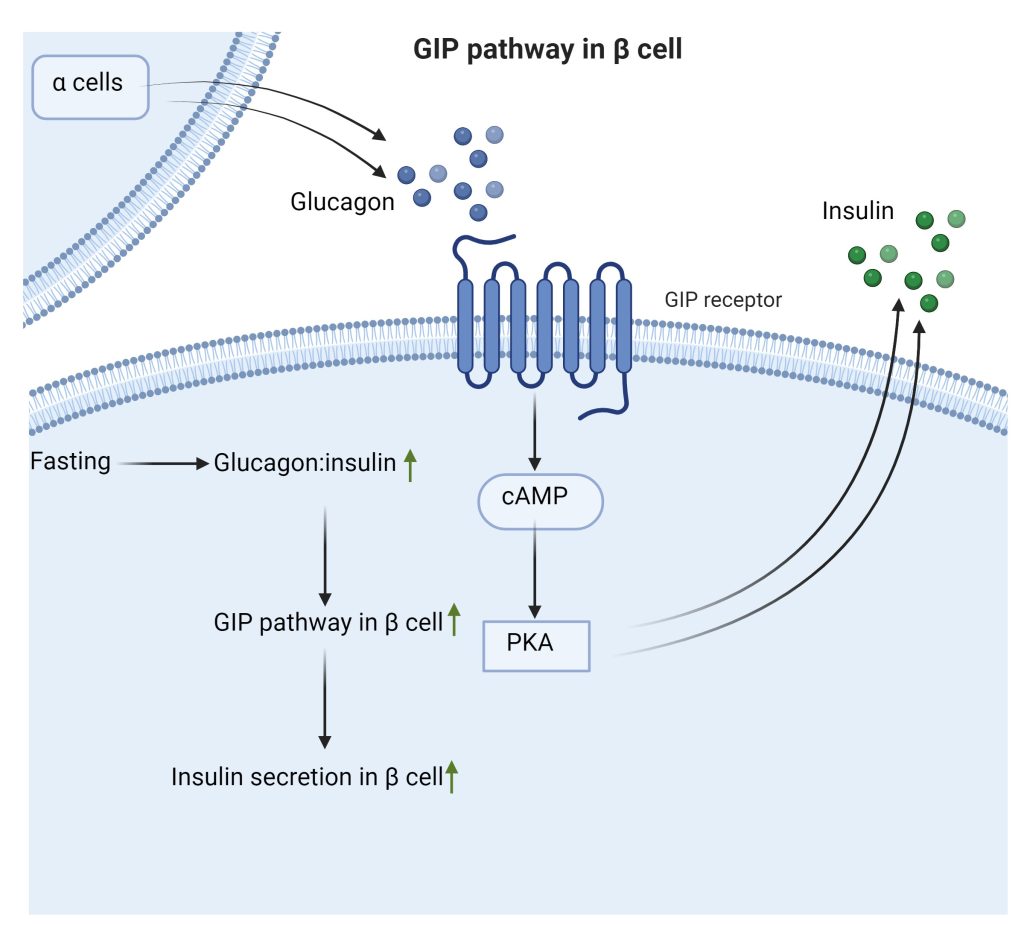
Free alanine, increased during periods of fasting or starvation, signals to the pancreas that blood glucose levels are low by stimulating glucagon secretion in α cells. Additionally, the glucagon secreted by α cells also contributes to the activation of the GIP receptor (GIPR) pathway in β cells, which release insulin after activation. GIP-stimulated glucagon secretion produces substantially more insulin secretion than what is achieved by GIPR activity in β-cells alone, by engaging in α-β cell communication.
Alanine-induced glucagon secretion, as displayed above in Figure 1, is comparable to glucose-stimulated insulin secretion. Therefore, free alanine produced for gluconeogenesis during periods of fasting induces a higher production of insulin during both high and low glucose states [19]. In summary, fasting-induced glucagon secretion (α-cells) will indirectly stimulate the release of insulin (β cell ) to allow cells to take in blood glucose. This α-β cell communication of the pancreas is a key example of the body’s ways to regulate blood glucose.
An intermittent fasting regimen would case an increase in alanine-induced glucagon secretion during the fasted state (Figure 2). Through α-β cell communication, insulin will be secreted to better prepare other tissues for uptaking glucose from the bloodstream. Inducing the fasted state will therefore impact glucose metabolism by increasing insulin production to more effectively lower blood glucose levels.
In summary, a time restricted eating regimen induces secretion of glucagon during periods of fasting. This hormone signals to mobilize glucose to the bloodstream, thus increasing blood glucose concentration. But how will this new glucose be taken into cells? Through communication between pancreatic cell types, glucagon also stimulates insulin to be secreted so that the newly mobilized glucose can be taken into the cells that need it. Overall, intermittent fasting improves glucose metabolism by influencing the secretion of two hormones that are essential for its homeostasis.
December 4, 2023 at 1:07 pm
Great information here too. All of your info so far has contributed well to the evidence for intermittent fasting. I noticed that glucagon nor insulin (was mentioned earlier on) was mentioned to be specifically a peptide hormone. It may be worth it to specifically mention at some point earlier, not necessarily here, how peptide hormones differ from other hormone types like steroids and amino acids. Mentioning how both of these molecules specifically act on cell membranes, produce fast effects in the body, and are composed of amino acids may provide some interesting context for the site as a whole. No true comments about this page specifically, I’ve found your graphics to be incredibly helpful so far.
December 5, 2023 at 2:15 am
I seriously do not understand how the diagrams are so aesthetically pleasing and well made (looks professionally done!). Each one not only looks great but also effectively communicates and reframes the information from the page without feeling repetitive. The page does an excellent job of establishing connections between the two pancreatic hormones, Glucagon and Insulin, and their roles in Type II diabetes. However, I’m a little confused about why the alanine-induced release of Glucagon through intermittent fasting is considered beneficial. In the Phosphorylation of cAMP response element-binding protein (CREB) page, it’s explained that type II diabetes leads to over-phosphorylation of CREB, resulting in elevated blood sugar levels. Since this phosphorylation is attributed to Glucagon, wouldn’t stimulating the release of glucagon through intermittent fasting be counterproductive for Type II patients? Some clarification on this point would work nicely!
December 13, 2023 at 6:48 pm
Hi Pun! Thank you so much for your compliments on the figures. 🙂
Also, I agree that this pathway can be a little confusing when thinking about the functions of insulin and glucagon. I added a paragraph at the very end of the page to summarize it in simple terms. Basically, intermittent fasting will improve glucose metabolism through communication between these two hormones. Since glucagon works to increase blood glucose, the secreted insulin will help prepare tissues to take it in.
I also added some more to the opening paragraph to explain that Type II diabetics might also have insufficient insulin secretion, which is where this pathway comes in.
December 5, 2023 at 4:47 pm
Your explanation on intermittent fasting/gluconeogenesis on improved insulin secretion was very clear, and I liked how you utilized the concept of gluconeogenesis to transition to alanine and its specific effects on alpha and beta cells to procure homeostasis. I also liked how you emphasized/reiterated the connection between alanine-induced glucagon secretion and intermittent fasting at the end once again, bringing all of this key information together. I noticed in the second paragraph you mentioned that blood concentrations of alanine and “other amino acids” increase during fasting. One small thing you might want to clarify is to preface the first sentence of the third paragraph by saying “Unlike other amino acids,” better highlighting alanine’s special capability in affecting alpha/beta cells, in comparison to other amino acids. Even providing a sentence about its potential structural advantage towards this phenomenon could be useful.
December 13, 2023 at 6:51 pm
Hey Andy! I like your note on adding “unlike other amino acids” to highlight the importance of alanine here. I changed this around and think it works well. Thank you for all of your feedback!
December 8, 2023 at 5:57 pm
Great page. I didn’t realize glucagon and insulin were so interconnected. A sentence explaining which tissues alanine is coming from would be beneficial so that the whole picture can be understood. In the third paragraph, you could combine the first and second sentences to make it read better by saying, “various hormones, including…” The flowchart and schematic are really nice and easy to follow! Finally, being more specific about what type of tissues respond to insulin or glucagon in this scenario would make the whole process easier to understand.
December 13, 2023 at 6:50 pm
Thank you Ezra!! I changed that sentence around a little from the first paragraph that you mentioned. I think it helps the flow of the writing without being too choppy. Thank you again for your comments!
December 10, 2023 at 5:19 pm
Continuously impressed with the work on this cite. As much as I thought I learned on carbohydrate metabolism, I did know there was so much more to uncover. The explanation on how free alanine ultimately results in insulin secretion and how intermittent fasting is involved is well done. As always, the figures look meticulously crafted to summarize the information presented in the paragraph in an appealing and concise manner.