Kenya Palmer Emrich, MS, MSN, FNP-BC, CSCS, NBC-HWC.
Nutrition Intervention, Communication, Behavior Change (NICBC)
My journey began with a childhood fascination for the human body and movement. My career in fitness and athletics drove me to help clients struggling with weight management. This led me to nursing school and an eight-year career in obesity medicine, focusing on behavior change in patients seeking care. Realizing the need for a formal theoretical foundation, I pursued nutrition studies.
I hold a BS in Rehabilitation Counseling and Nursing and an MS in Exercise Science and Nursing. I have worked in fitness, athletics, strength training, and obesity medicine. I am a full-time nursing instructor and a part-time Nutrition and Wellness Coach and Movement Specialist.
I am interested in mixed-methods research in behavior change, lifestyle management, cardiometabolic disease, obesity, and health disparities, focusing on African American women and girls and the mother-daughter dyad. I am particularly interested in the intersections of artificial intelligence within these areas, utilizing a mixed-methods approach.
Final Presentation
Final Project
Artificial Intelligence and Health of U.S. Military Veterans Future implications in Food Insecurity
Project Description
Abstract: Obesity is the most significant global chronic non-communicable disease. Efforts to address obesity within the African American community, especially among women and girls, have been largely ineffective. Artificial intelligence (AI) and machine learning (ML) tools have been used to identify those at risk for obesity. There is limited research on AI/ML in obesity and AA communities. This six-month prospective observational study explores the potential of AI/ML tools to identify obesity risk factors and develop effective targeted interventions for AA women and girls, specifically within mother-daughter dyads (MDD). This research aims to (1) Utilize AI/ML to identify and predict obesity risk factors in this population, (2) apply AI/ML-driven models to develop interventions grounded in behavior change theory, and (3) determine if the interventions help decrease obesity within this population.
Key Words: Artificial Intelligence (AI), Machine Learning (ML), obesity, behavior change, prediction, African-American, Mother-Daughter dyad.
Introduction & Rationale: Despite various interventions, including individualized home approaches, medical-surgical interventions, and public policy, obesity rates have continued to rise in the US for over 40 years, especially among AA women and girls. Research highlights the influence of the mother-daughter dyad on health behaviors and obesity, yet more targeted approaches are needed. Integrating AI/ML in research offers innovative opportunities to address obesity in AA women and girls through the MDD. Thus, the rationale for this work is to fill ongoing knowledge gaps regarding risk factors that heavily influence the intergenerational obesity rates in this population and then create targeted culturally specific interventions based on behavior change theory, to decrease obesity prevalence.
Literature Review:
Obesity is a chronic relapsing disease associated with other health complications, social bias and stigma, and physical disability, affecting adults and children throughout the world. Despite ongoing research in obesity medicine, non-Hispanic Black women and girls continue to see obesity increase in their communities, suggesting interventions are woefully ineffective (Hayba et al., 2020). In the United States, over 70% of the adult population and approximately 35% of children are overweight or have obesity (NIDDK, 2021). Of those affected by the disease, non-Hispanic Black women and girls have the most significant prevalence, 56.9%, and 29.1%, respectively (NIDDK, 2021). The AA mother-daughter dyad (AA-MDD) has shown to be a powerful resource for change in health behaviors, especially in cancer research; however, this duo has yet to be the target in interventional obesity research. Strategies have been identified (Reed et al., 2017), but little research has applied these strategies utilizing behavior change theory in a targeted and culturally specific manner.
Contributing to the growing research on obesity is crucial, especially in the AA-MDD. Machine learning research in obesity is increasing (DeGregory et al., 2018), and considering the gaps in obesity research among this population, it is possible that AI/ML can be a beneficial tool. Artificial intelligence and ML, used in obesity research (Cheng, Steinhardt, & Ben Miled, 2022), could be leveraged to help identify risk factors to improve and apply targeted, culturally appropriate interventions for the AA-MDD. The following Use Case Description addresses these research deficits and explores the possibilities of AI/ML utilization.
Use Case Description
Objective(s) of the use case: The primary aim of this use case is to provide insight into how AI/ML can contribute to the growing research knowledge of AA-MDD and obesity by addressing the following objectives and aims of this study:
Objective 1: Predicting obesity in AA women and girls and the AA-MDD
Aim #1: Utilize AI/ML models to identify and predict risk factors in this population
Objective 2: Apply Behavior Change Interventions
Aim #2: Utilize AI/ML models to develop targeted, culturally specific interventions based on behavior change theory
Objective 3: Measure weight change
Aim #3: Evaluate the effectiveness of AI/ML-informed interventions in improving health behaviors and decreasing obesity in the AA mother-daughter dyad.
Methodology/Approach: To meet the first objective and aim of this study, a 6-month prospective observational study of AA-MDDs utilizing surveys, medical records, wearable devices, and environmental assessments to identify significant obesity risks in AA women, girls, and AA-MDD using AI models. Risk factors will then be categorized to predict obesity within the community, utilizing ML models. Results from the initial study can then be used to create targeted, culturally appropriate behavior change interventions based on the Socio-ecological. Once targeted interventions are implemented, long-term goals of decreasing obesity prevalence.
Key Stakeholders: Our most important stakeholders are the AA women and mothers who comprise the MDD, who must be at the center of every decision made throughout the project. If considering the socio-ecological model of behavior change, other vital stakeholders include family members and other members within the AA communities. Additionally, local, state, and federal policymakers are essential stakeholders to leverage in the future. Lastly, AI/ML is a recognized stakeholder as it builds its knowledge base and continues to learn as we create and provide research.
Proposed AI techniques or tools: Identifying the most effective AI/ML method to utilize for this research is crucial to its success, contribution to the growing literature on obesity and AI/ML and addressing the aims of this study. Some methods are most effective at prediction, and others are most effective at describing or characterizing the data gathered (DeGregory et al., 2018). The latter is more equipped to find relationships between many variables. Decision tree learning, a type of machine learning, has been used to predict childhood obesity (DeGregory et al., 2018). The decision tree approach is optimized by using random forests to aggregate data and create a more predictive model (DeGregory et al., 2018). Random forest ML analysis will identify the most significant risk factors impacting weight gain, including social determinants of health (SDOH).
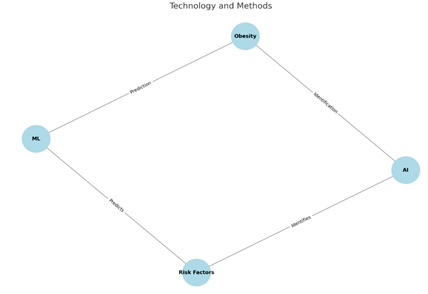
Knowledge Graphs, Conceptual Maps, and Causal Diagrams:
To effectively address the rising prevalence of obesity in AA-MDD, a glossary of terms (Appendix A) must be created. The relationship between these terms promotes a working understanding of the language and provides clarity and direction for this research. Additionally, drawing relationships between the central concept (obesity) is essential to understanding the overall impact on the research.
Ethical Considerations:
Conducting AI/ML research on underrepresented communities like AA women and girls involves several ethical considerations: beneficence and maleficence, fairness and equity, transparency and accountability, informed consent and privacy, human centricity, and cross-cultural sensitivity. Health and nutrition research bias often negatively impacts underrepresented populations, which can be exacerbated in AI/ML research. Ethical considerations must be leveraged to protect the communities, including transparency, accountability, informed consent, and privacy, to mitigate and prevent algorithmic and ongoing racial and ethnic biases. Given the known concerns of research with children and women, this research will utilize frameworks like ACCEPT-AI and Women4Ethical AI. These frameworks are essential to avoid existing racial biases in healthcare algorithms (Muralidharan, Burgart, and Daneshjou, 2023) and advancing gender equity (UNESCO, n.d). Conclusion and Recommendations: This research underscores the value of AI/ML tools in addressing rising obesity prevalence among AA women and girls within the AA-MDD. By leveraging AI/ML to identify and predict obesity risk factors and develop targeted, culturally specific interventions grounded in behavior change theory, this research will fill critical knowledge gaps and provide innovative solutions to reducing obesity prevalence in this population. The integration of AI/ML offers a promising avenue for personalized and effective obesity interventions, a crucial step toward overcoming historically ineffective strategies used in the AA community.
Appendix: Glossary of Terms
| Adult | Person AMAB or AFAB chronologically at the age of 20 or older, as defined by NHANES (national Health and Nutrition Examination Survey). | |
| Women | Person AFAB. Can include transgender male, non-binary, cisgender female. Based on chronological age and not puberty. Age of 20 years or older. | |
| Mother | A person, regardless of age, that has conceived (naturally, through IVF or surrogacy), adopted a child or has become a mother through marriage/relationship for at least 2 years. 2 years is defined as the cutoff because NHANES data is gathered on children, pediatrics above the age of 2. This limitation is necessary for a study evaluating obesity risk and interventions in mother-daughter dyads. | |
| African American | Any person that identifies as African American, regardless of birthplace or ancestorial lineage. May include a person of mixed ancestorial heritage. | |
| African | Any person who identifies as the following: born in Africa, born of parents from Africa, or known heritage from Africa or the African Diaspora. | |
| American | Any person who identifies as the following: born in America and/or its territories immigrated to the country and has nationalized, assimilated, or secured green card. Census data will not be determined for this study as it is beyond the scope of the research. It is not a characteristic modifiable through this study. | |
| Artificial Intelligence (AI) | Computer systems with the ability to imitate human intelligence and behaviors including learning, reasoning, problem solving, understanding language, and perception. Can be divided into subgroups including machine learning (ML), deep learning (DL) and natural language processing (NPL). | |
| Machine Learning (ML) | A subset of AI that involves the development of algorithms and statistical models that enable computers to improve their performance on tasks through experience. ML models learn from data to identify patterns and make predictions or decisions without being explicitly programmed for each task. ML models can be further divided into three categories: Supervised learning (SL), Unsupervised learning (USL) and Reinforcement learning (USL). | |
| Supervised Learning (SL) | Utilization of ML-AI to work with labeled data to make predictions or classifications. Examples: image recognition, speech recognition, and medical diagnosis. | |
| Body Mass Index (BMI) | The ratio of weight (wt) in kilograms (kg) to height (ht) in meters-squared (m2), used as a rough estimation of body fatness which is related to disease risk, including obesity. There are 5 categories used in adults (ages over 18) and 3 categories used in pediatric patients (2 – 18 years of age). Adult BMI cutoffs: Under Weight: </= 18.49kg/m2 Normal Weight: 18.5 – 24.9 kg/m2 Over weight: 25 – 29.9 kg/m2 Obesity: Obesity Class 1 30 – 34.9 kg/m2 Obesity Class 2 35-39.9 kg/m2 Obesity Class 3 40+ kg/m2 Pediatric BMI cutoffs: Normal weight: 5th -85th% Overweight: 85th – 95th% Obesity: > 95th% Severe obesity: 120% of 95th% or 35+ kg/m2. | |
| Mother-daughter Dyad | Any relationship between a mother and daughter. | |
| Obesity | Defined by BMI (see BMI above). A chronic non-communicable disease associated with cardiometabolic disease, morbidity and mortality. | |
| Obesity risk factors | There are several risk factors (modifiable and non-modifiable) that are known to increase the | |
| Modifiable Risk Factors | Modifiable risk factors are those that can be altered by the individual to prevent, slow progression of or treat obesity. Modifiable risk factors include: EpigeneticsPhysical inactivityExcessive caloric intakeIntrauterine environment Postnatal influencesInsufficient sleepMedication inducedMedical conditionsPsychosocial stressEndocrine disrupting chemicalsGastrointestinal microbiome Reference: Masood, B and Moothy, M. (2023). Causes of obesity: a review. Clinical Medicine. 23 (4): 294-291. DOI: 10.7851/clinmed.2023-0168 | |
| Child | Person AMAB or AFAB chronologically at the age of 19 years or younger, as defined by NHANES (national Health and Nutrition Examination Survey). | |
| Girls | Person AFAB. Can include transgender male, non-binary, cisgender female. Based on chronological age and not puberty. Age of 19 years or younger. | |
| Daughter | A person, regardless of age, born of a “woman” and has held a relationship for at least 2 years. 2 years is defined as the cutoff because NHANES data is gathered on children, pediatrics above the age of 2. This limitation is necessary for a study evaluating obesity risk and interventions in mother-daughter dyads. |
References:
Cheng ER, Steinhardt R, Ben Miled Z. (2022). Predicting Childhood Obesity Using Machine Learning: Practical Considerations. BioMedInformatics. 2022; 2(1):184-203. https://doi.org/10.3390/biomedinformatics2010012. Retrieved: June 2024.
DeGregory, KW, Kuiper, P, DeSilvio, T, Pleuss, JD, Miller, R, Roginski, JW, Fisher, CB, Harness, D, Viswanath, S, Heymsfield, SB, Dungan, I and Thomas, DM. (2018). A Review of Machine Learning in Obesity. Obesity Reviews, 19: 668-685. DOI: https://doi.org/10.1111/obr.12667. Retrieved: June 2024.
Hayba N, Elkheir S, Hu J, and Allman-Farinelli M (2020). Effectiveness of Lifestyle Interventions for Prevention of Harmful Weight Gain among Adolescents from Ethnic Minorities: A Systematic Review. International Journal of Environmental Research and Public Health. 17(17):6059. https://doi.org/10.3390/ijerph17176059. Retrieved: June 2024.
Muralidharan, V., Burgart, A., and Daneshjou, R. (2023). Recommendations for the use of pediatric data in artificial intelligence and machine learning ACCEPT-AI. npj Digit. Med. 6 (166). Retrieved from: https://www.nature.com/articles/s41746-023-00898-5. Retrieved: June 2024.
National Institute of Diabetes and Digestive and Kidney Disease, NIDDK (2021). Overweight and Obesity Statistics. Retrieved from: https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity. Retrieved: June 2024.
Reed, M, Julion, W, McNaughton, D and Wilbur, J. (2017). Preferred intervention strategies to improve dietary and physical activity behaviors among African-American mothers and daughters. Public Health Nursing, 34(5): 461-471. Doi: https://doi.org/10.1111/phn.12339. Retrieved: June 2024.




Hi Kenya,
I appreciated your transparency regarding the bias you encountered while developing this work and providing specific ethical frameworks to address research concerns. Using AI to contribute to research on AA-MDD and obesity could support meaningful change. I look forward to seeing the positive impact of your proposed study.
Hi Kenya, awesome job! Your project addresses an important topic and has an interesting design. It’s exciting to think how AI can enhance traditional study designs – like your suggested prospective cohort study. It would also be interesting to see how AI can handle the complex interactions between the factors that contribute to obesity risk in the mother daughter dyad (from personal/biological/behavioral to enivornmental/community/cultural).
P.S I am going to check out ACCEPT-AI and Women4Ethical AI. Thanks for including these!
Hi Kenya, you did a wonderful job providing a Glossary of Terms. I’m excited to see your work on predicting the population and implementing behavior change models. The logic is very clear. Could you elaborate on how your methodology plans to account for and preserve the cultural integrity and personal preferences of the participants while implementing these interventions?
Your causal diagram does a powerful job of outlining the relationship between obesity, it’s risk factors and interventions. I believe that this research is incredibly important to do exactly what you said, fill the holes in an already lacking nutrition research space. Using AI effectively could very well be exactly what’s needed to lower the barrier to adequate research and substantial analyses.
Hi Kenya,
Your project ended up very informative and I appreciate how you outlined the current limitations of using AI in your research. However, I am curious as to how you plan to train a LLM to better help with this research topic? What datasets do you think would be the most useful in the training process? Would you consider a supervised or an unsupervised approach? I look forward to your dissertation results!
Hi Kenya, wonderful job! I’m particularly impressed by your integration of various data sources, like medical records and wearable device data, which are essential for developing accurate and actionable AI models. Your use of decision tree learning and random forests to refine predictions and categorize risk factors is a great demonstration of applying machine learning techniques in real-world health scenarios.
Hi Kenya, I believe that this is a very important topic and I am excited to see where your research heads! Because the data in this area is currently limited, I am curious to see how AI/ML will be impacted by data limitations and if predictive models will be skewed because of these limitations. Do you think that AI would be able to overcome current biases related to obesity and health in AA-MDD or would it be necessary to have significant human oversight to ensure cultural relevance and sensitivity?