John E. Rush, DVM, MS, DACVIM (Cardiology), DACVECC
Cummings School of Veterinary Medicine at Tufts University
OBJECTIVES
- If necessary, review from prior classes the physiology associated with myocyte activation, depolarization, and restoration of ionic gradients. These concepts will be needed in order to understand ECG interpretation, arrhythmia formation, and the mechanism of action for antiarrhythmic and inotropic drugs. Specifically review:
- Excitation permeability changes
(Na+ and K+) and the role of the Na-K pump.
- The role of spontaneous (phase 4) diastolic depolarization in cardiac tissues which demonstrate the property of automaticity (pacemaker activity) such as the SA node, the AV junctional tissue, and the Purkinje fibers in the ventricle.
- Phases of the action potential (Phases — 0, 1, 2, 3, 4).
- The electrical activation of the heart which leads to the P, QTS, and T waves.
- Understand the concepts of tissue excitability, the refractory periods, conduction velocity in different tissues, automaticity.
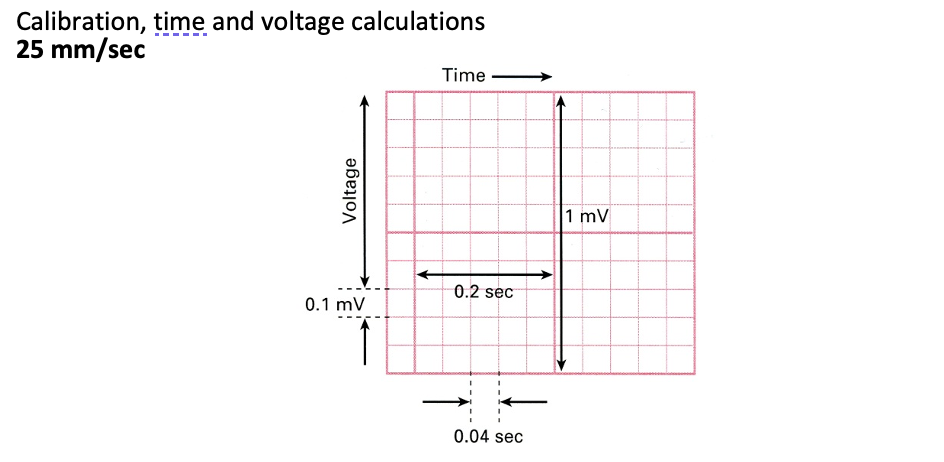
- Know normal values for heart rate, P wave height and duration, QRS height and duration, P-R and Q-T intervals, and be able to calculate these values from ECGs recorded at 25 and 50 mm/sec, 1 cm/mv in dogs, cats, horses and cattle.
- List three potential advantages for use of precordial electrocardiographic leads.
ELECTROPHYSIOLOGIC CONSIDERATIONS
1. Review of the impulse-forming and conduction system in the SA node, interatrial pathways, A-V node, A-V junction, Bundle of His, Bundle branches, Fascicles and Purkinje system.
2. Review the transmembrane (action) potential of two types of cells – an “Automatic” or pacemaker cell and a ventricular myocardial cell.
a. Note the pacemaker cell exhibits spontaneous (phase 4) depolarization and can “drift” to the threshold potential at which point spontaneous depolarization occurs.
b. Depolarization waves are propagated through the conduction system and myocardium resulting in the electrical-mechanical interactions responsible for myocardial pumping functions.
3. Normally, the S-A node is the dominant pacemaker; however, cells in the atria, A-V junctional tissue and His-Purkinje system have “automatic” properties. The shape of the action potential varies among these tissues and partially accounts for the hierarchy of pacemakers. The more rapid rate of discharge of the SA node tends to keep other pacemakers suppressed (overdrive suppression). The action potential of one group of pacemaker cells may change, however, so that the SA node may lose its dominant role in controlling heart rate (suppression) or other automatic tissues may have enhanced function such that they take control of the heart rhythm (usurpation). If either of these occurs, the dominant pacemaker focus may change resulting in arrhythmia.
4. Excitability refers to the ability of cardiac tissue to be depolarized by a stimulus. The pericardium and cardiac valves are not excitable. However, excitable tissues are not excitable during a relative or absolute refractory period. This property normally assists in preventing unusual pacemakers from usurping the dominant pacemaker role.
5. The conduction velocity through any given tissue depends upon the quality (shape) of its action potential and the time in the cardiac cycle at which it is stimulated. Conduction through the AV node is very slow, while conduction through the bundle branches and Purkinje fibers is much faster. Tissue in a refractory state cannot propagate an impulse from any source. Examples of conduction velocity: SA node 0.02 – 0.1 m/sec; Purkinje fibers 1-4 m/sec.
6. Dysrhythmias result from abnormal electrical activity. Dysrhythmias also lead to further electrical instability. Several factors may contribute to arrhythmia formation, including:
a. Changes in automaticity – either suppression of the dominant pacemaker (e.g. vagal tone suppresses SA nodal automaticity) or enhancement of other pacemaker tissues (e.g. from disease or by drugs).
b. Impaired conduction – blockage of impulses and/or decreased velocity of conduction through certain myocardial tissue (e.g. digitalis slows A-V nodal conduction). This normally occurs to some degree in the A-V node and is termed decremental conduction. However, if this occurs in the atrium, junction or ventricle, roundabout circus or reentrant pathways may be set up, leading to extrasystoles.
c. Inhomogeneity of refractoriness may be an important factor in arrhythmogenesis including reentry and myocardial fibrillation.
8. Changes in automaticity and conduction are brought about in a number of ways and different drugs and conditions are capable of initiating or suppressing dysrhythmias and conduction disturbances. Refer to Fig. 1. Potential sites of action include the:
a. Resting transmembrane potential
b. Threshold potential
c. Rate of rise of the action potential (AP)
d. Duration of the AP
e. Rate of rise of phase 4 depolarization
Definitions (know ones in bold):
Arrhythmias can be defined as any abnormality in the rate, regularity, site of origin or conduction of the cardiac impulse such that the normal sequence of atrial and ventricular activation is altered.
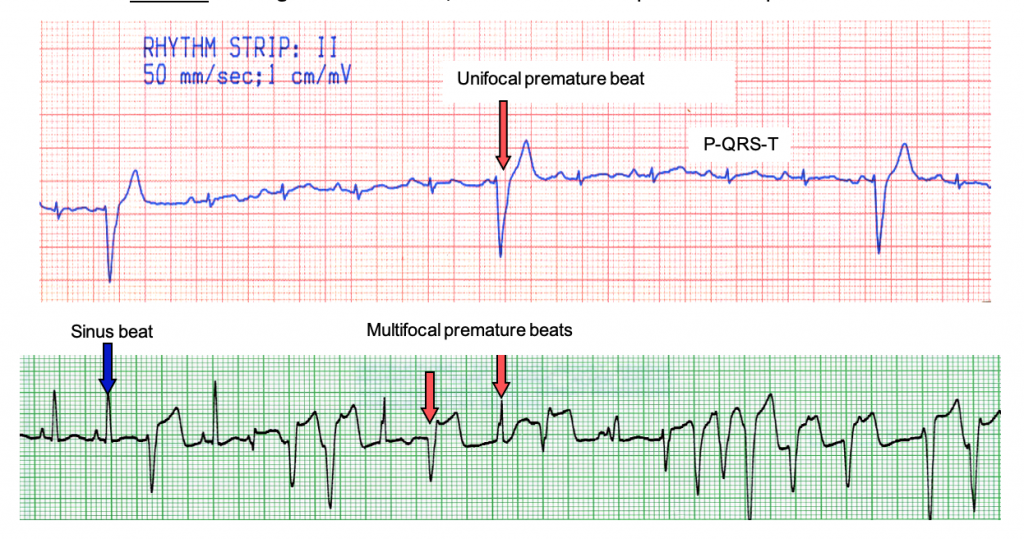
1. Ectopic – an impulse arising in any focus other than the S-A node. Ectopic discharges result in abnormal configurations of the P-QRS-T complex.
2. Extrasystole – a premature, ectopic depolarization dependent on and coupled to the preceding normal beat, but originating from an ectopic focus.
3. Parasystole – an independent, ectopic rhythm operating alongside the dominant pacemaker, but “protected” from depolarization by the dominant pacemaker. It causes an ectopic depolarization if it discharges during a period when the heart is not refractory. The ectopic depolarizations are not coupled to the previous QRS by a fixed time interval.
4. Premature depolarization – an ectopic impulse which follows the preceding P or QRS by an interval which is shorter than the predominant normal P-P or R-R interval.
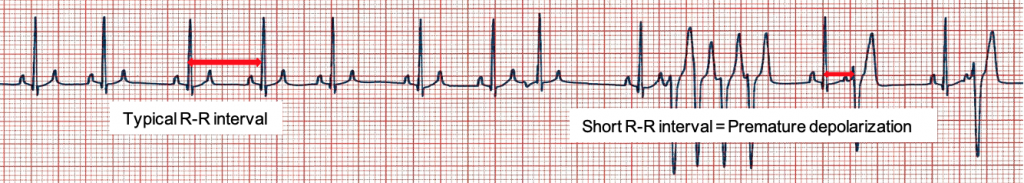
5. Escape depolarization – an ectopic depolarization “late” after the dominant pacemaker has failed to initiate a systole during its normal cycle length (normal R-R interval).

6. Conduction block – a pathologic delay or interruption of conduction.

7. Coupling – the relationship between an extrasystole and the complex preceding it. It is felt that the preceding complex sets up the conditions that allow the extrasystole to occur (e.g. by inciting a local conduction block).

8. Compensatory pause – the pause that follows an extrasystole which does not depolarize (reset) the SA node, therefore, the next normally conducted QRS falls in line with the previous rhythm. The R-R interval of the two normal complexes surrounding the premature complex is exactly twice the normal R-R interval (or P-P interval).
9. A-V dissociation – independent depolarization of atria and ventricles; usually associated with abnormal A-V conduction or ectopic ventricular rhythms.

10. Ventricular capture – a normally conducted QRS following a period of A-V dissociation.
11. Fusion – a complex formed when a normally conducted impulse and a ventricular ectopic pacemaker simultaneously depolarize the ventricle. It is intermediate in appearance when compared to the ventricular extrasystole and the normally conducted impulse. A sign of A-V dissociation.

12. Aberrant ventricular conduction – abnormal spread of supraventricular impulse through the ventricles. Abbreviated as AVC.
13. Retrograde conduction – reverse impulse propagation through the conduction system (e.g. from ventricle to atrium); not common in animals.
14. Interpolation – a premature complex that occurs between two normal beats without disrupting the rhythm.
15. J point – the beginning of the ST segment.
16. Paroxysmal tachycardia – “burst” of tachycardia; a sudden onset and abrupt end.

17. Unifocal – arising from one source, as with ventricular premature depolarizations.
18. Pre-excitation syndromes – when the ventricles are excited prematurely due to an abnormal (faster) A-V conduction pathway. One example is the W-P-W syndrome (Wolfe-Parkinson-White).
19. Fibrillation – chaotic, disjointed, mosaic myocardial activation

ELECTROCARDIOGRAPHY PHYSIOLOGY BASICS
Autonomic effects on pacemaker cells
1. Parasympathetic stimulation decreases HR
a. Rate of diastolic depolarization decreased.
2. Sympathetic stimulation (e.g., norepinephrine) increases HR
a. increases slope of phase 4, speeds rate of diastolic depolarization
SA and AV nodes
The SA node, possessing the highest inherent automaticity, normally acts as the pacemaker for the heart and the autonomic nervous system can increase the heart rate (positive chronotropism) or decrease heart rate (negative chronotropism) but the sympathetic system is obviously not necessary for initiating the heartbeat. The major direct effects of the parasympathetic nervous system on the heart are at the SA and AV nodes, which slow heart rate and AV conduction, respectively. Increased parasympathetic activity also tends to modestly depress atrial contractility and ventricular contractility (inotropic state).
The AV node is situated within the interatrial tissue, near the ventricles. The nodal region cells anatomically and functionally resemble those of the SA node in most respects. The AV node has several functions: 1) it is a conduction bridge between the atrial and the ventricles, 2) it induces a delay between atrial and ventricular depolarization, 3) it is a backup pacemaker for cells within the AV node (i.e., junctional region cells have pacemaker potential that can initiate the heart beat in the absence of appropriate SA node firing). The AV node cannot conduct very rapidly, and in some instances, it acts as a “protector” when the atrial rate gets exceedingly rapid, in that every impulse may not pass through the node so the ventricles do not beat as rapidly. With pathology of the region, the AV node may not conduct every impulse even when the atrial rate is slow and this is known as second or third degree atrioventricular block.
THE ELECTROCARDIOGRAM
Electrodes, leads, in clinical ECG (synonymous with EKG)
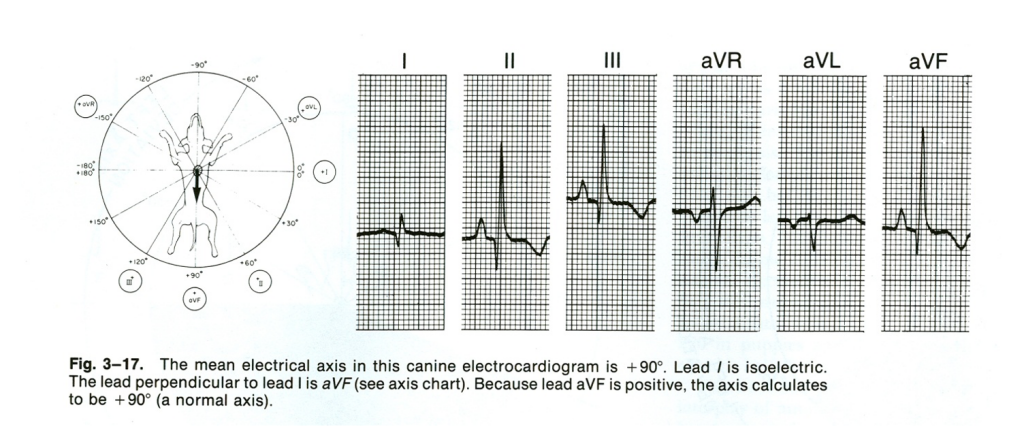
1. Standard limb leads: I, II, III
2. Augmented unipolar limb leads: aVR, aVL, aVF
3. Unipolar chest (V) leads: V1 – V6
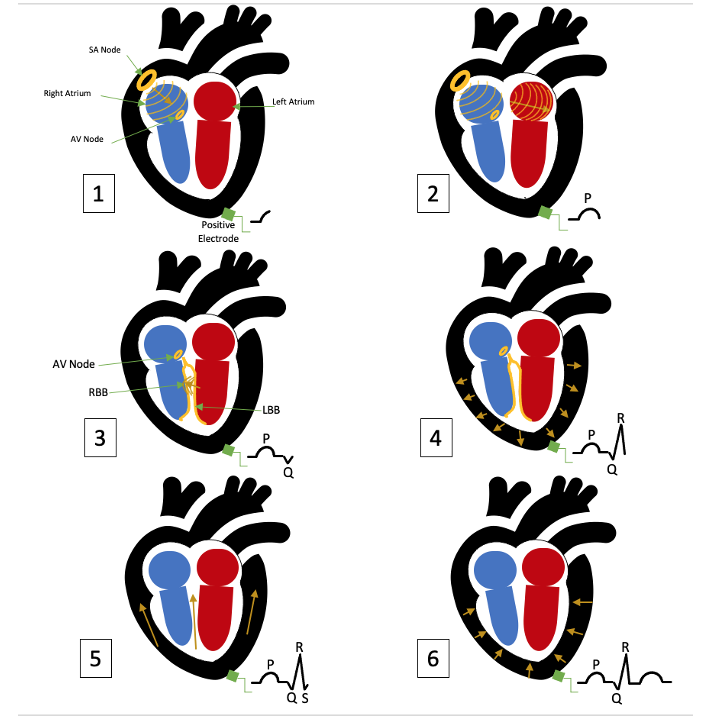
Variation of Ventricular Activation between species
1. Category A — dog, cat, man, monkey, rat — subendocardial Purkinje fibers only
a. Initial (5-10 msec of QRS) endocardial shell surrounding apex of LV (simultaneous depolarization of IVS from R–L). Result small vector from L — R, “q” wave in some
b. Depolarization of both ventricular “free walls” (next 15-20 msec) from endocardium to epicardium. Results in large vector toward LV normally — “R” wave in a VF
c. Terminal (5-10 msec of QRS) from depolarization of the bases of the ventricles and septum. Result in small vector, apicobasilar direction, “S” wave in some leads.

2. Category B (hoofed mammals, dolphins) — horse, cow, pig, sheep, goat — characterized by Purkinje fiber penetration of myocardium to the epicardium.
a. Initial “shell” as in A animals above (15 msec)
b. Major mass of ventricles depolarized with “burst” of activation in many directions because of Purkinje penetration — results in little contribution to QRS because of cancellation — no “resultant vector”
c. General apicobasilar “mean vector” to QRS results (ventrodorsal) often slightly to right, contribute to QRS mainly from early and late forces, with major portion of ventricular wall depolarization “cancelled.”


Normal Electrocardiographic PQRST Criteria in Dogs and Cats
1. Representative lead II PQRST complexes in a dog and a cat (50 mm/sec, 1cm = 1mv)
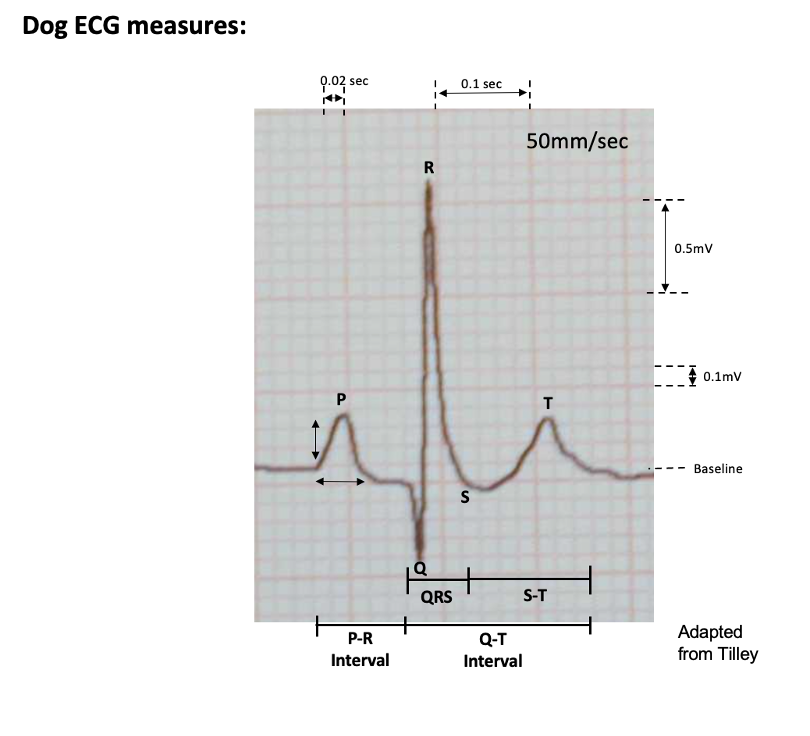
2. Standard nomenclature: measurements are taken at paper speed = 50 mm/sec and calibration setting of 1cm = 1mv, or paper speed = 25 mm/sec and calibration setting of 1cm = 1mv.
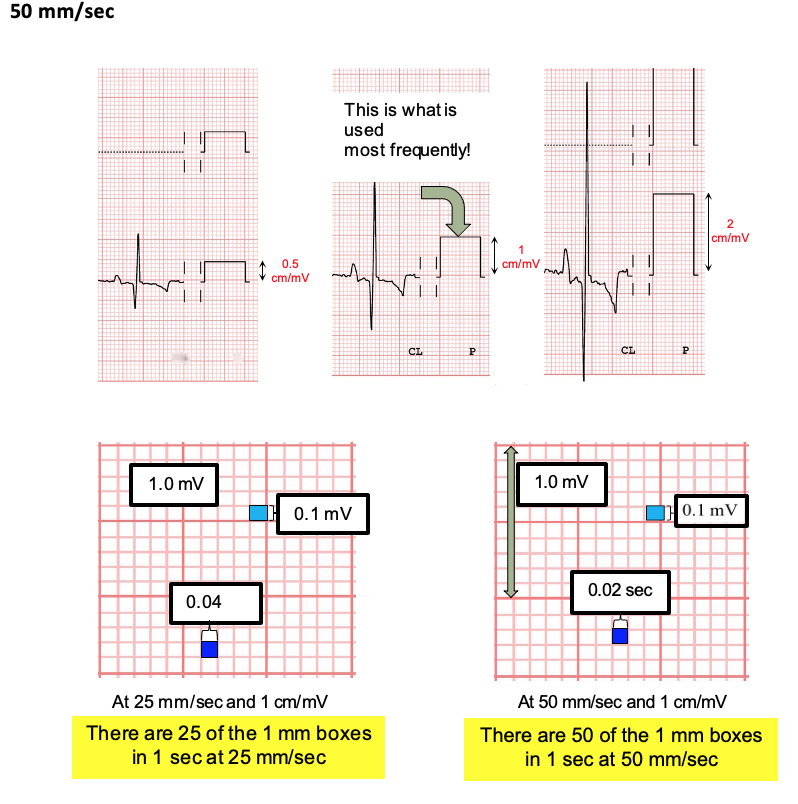
3. Representative calibration effects on PQRST amplitudes:

4. Dog Normal values
- Rate:
- 70 to 160 beats/min for adult dogs
- Up to 180 beats/min for toy breeds
- Up to 220 beats/min for puppies
- Rhythm:
- Normal sinus rhythm
- Sinus arrhythmia
- Wandering SA pacemaker
Measurements (lead II, 50 mm/sec paper speed, 1cm = 1mv):
- P wave:
- Width: maximum, 0.04 second (2 boxes wide)
- Height: maximum, 0.4 mv (4 boxes tall)
- P-R interval: Width: 0.06 to 0.13 second (3 to 6 1/2 boxes)
- QRS complex:
- Width: maximum 0.05 second (2 1/2 boxes) in small breeds, maximum 0.06 second (3 boxes) in large breeds
- Height of R wave*: maximum 3.0 mv (30 boxes) in large breeds, maximum 2.5 mv (25 boxes) in small breeds
- S-T segment:
- No depression: not more than 0.2 mv (2 boxes)
- No elevation: not more than 0.15 mv (1 1/2 boxes)
- T wave:
- Can be positive, negative or biphasic
- No greater than one fourth amplitude of R wave
- Q-T interval:
- Width: 0.15 to 0.25 second (7 1/2 to 12 1/2 boxes)
- shorter Q-T intervals and vice versa
- Electrical axis (frontal plane): + 40° to + 100°
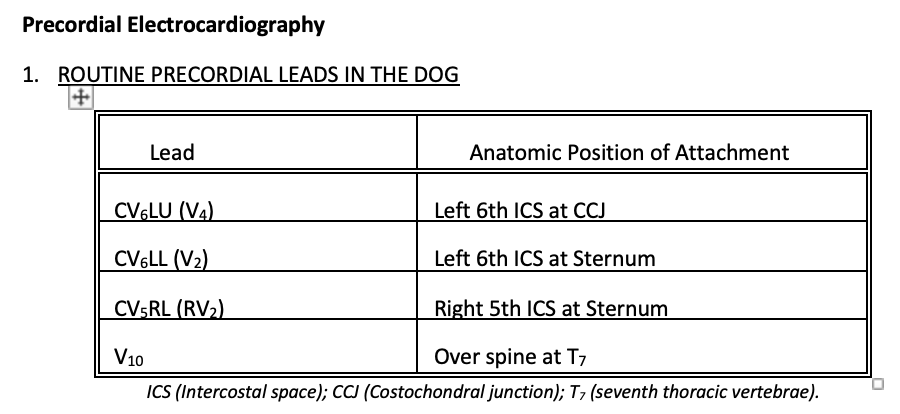
Precordial chest leads (values of special importance):
- CV4RL (rV2): T wave positive
- CV6LL (V2): S wave not greater than 0.8 mv (8 boxes), R wave not greater than 2.5 mv (25 boxes)*
- CV6LU (V4): S waves not greater than 0.7 mv (7 boxes), R wave not greater than 3.0 mv (30 boxes)*
- V10: negative QRS complex, T wave negative except in Chihuahua
*Not valid for thin deep-chested dogs under 2 years of age.
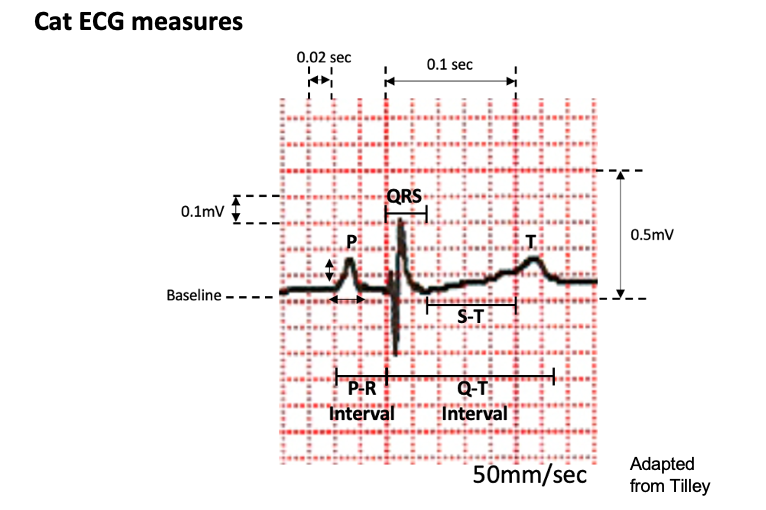
5. Cat Normals
- Rate
- Range: 160 to 240 beats/min (with excitement)
- Mean: 197 beats/min
- Rhythm
- Normal sinus rhythm
- Sinus tachycardia (physiologic reaction to excitement)
Measurements (lead II, 50mm/sec, 1cm=1mv)
- P wave:
- Width: maximum, 0.04 second (2 boxes wide)
- Height: maximum, 0.2 mv (2 boxes tall)
- P-R Interval:
- Width: 0.05 to 0.09 second (2 1/2 to 4 1/2 boxes)
- QRS Complex:
- Width: maximum, 0.04 second (2 boxes)
- Height of R wave: maximum, 0.9 mv (9 boxes)
- S-T segment: No marked depression or elevation
- T wave:
- Can be positive, negative or biphasic, most often positive
- Maximum amplitude: 0.3 mv (3 boxes)
- Q-T interval:
- Width: 0.12 to 0.18 second (6 to 9 boxes) at normal heart rate (range 0.07 to 0.20 sec, 3 1/2 to 10 boxes); varies with heart rate (faster rates, shorter Q-T intervals and vice versa)
- Electrical axis (front plane): 0 to + 160o
- Precordial chest leads: CV6LU (V1): R wave not greater than 1.0 mv (10 boxes)
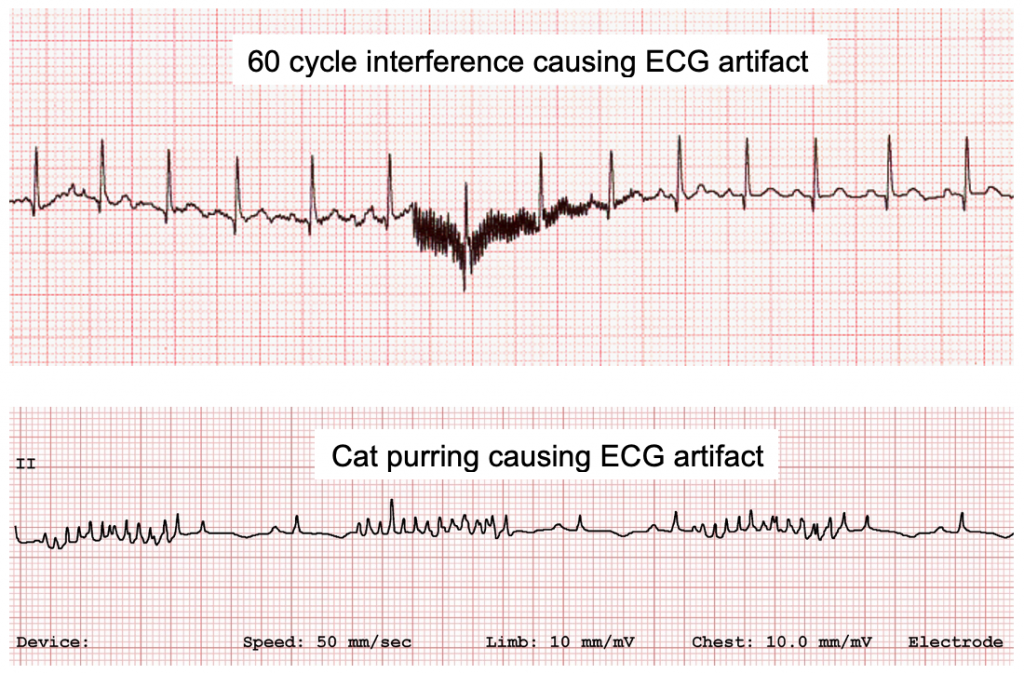
6. Artifacts: Artifact is fairly common on ECG in the living, breathing patient. Some examples of potential artifacts are shown below.

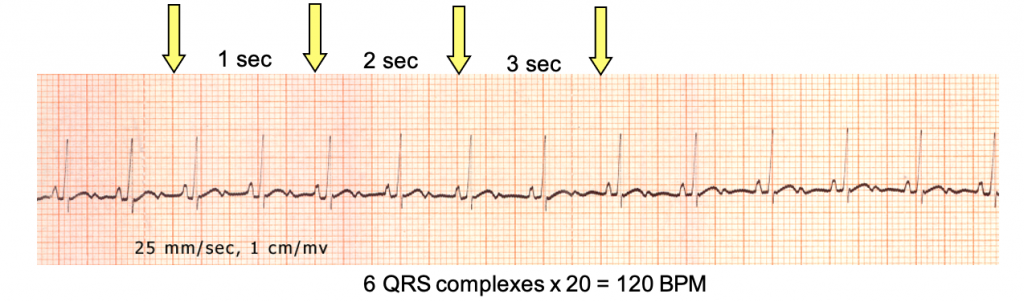
6. Calculating Heart Rate
a. Method 1
- 50mm/sec: 50 little boxes/sec; 10 big boxes/sec
- Count # of QRS in 3 seconds
- Multiply by 20 to get HR

- 25mm/sec:
24 little boxes/sec; 5 big boxes/sec
- Count # of QRS in 3 seconds
- Multiply by 20 to get HR
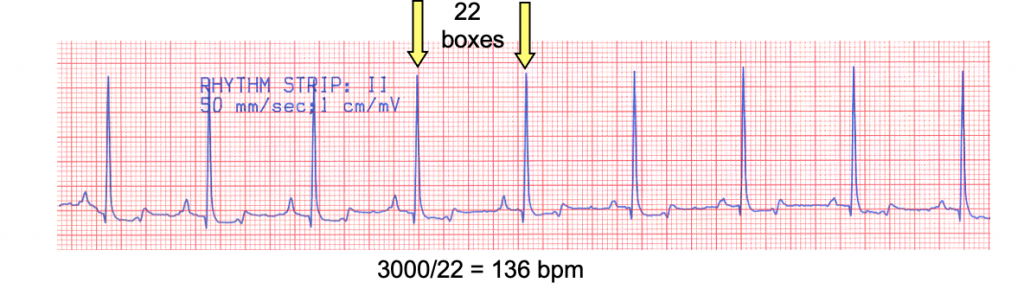
b. Method 2
- 50mm/sec
- Count # of boxes between R waves
- Divide into 3000 to get HR
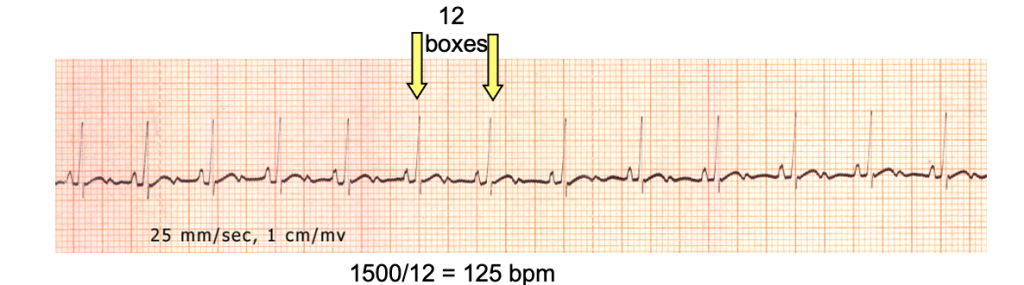
- 25mm/sec
- Count # of boxes between R waves
- Divide into 1500 to get HR

Vectors and generation of surface ECG potentials
1. Relationship of lead configuration to wave front vector detected by surface ECG.
a. A diagrammatic way to consider waves of depolarization

2. Normal electrical activation of heart
Configuration of Limb Leads for the Frontal Plane
Bipolar standard leads
Lead I – right arm (-) compared with left arm (+)
Lead II – right arm (-) compared with left leg (+)
Lead III – left arm (-) compared with left leg (+)
Augmented unipolar limb leads
Lead aVR – right arm (+) compared with left arm and left leg (-)
Lead aVL – left arm (+) compared with right arm and left leg (-)
Lead aVF – left leg (+) compared with right and left arms (-)

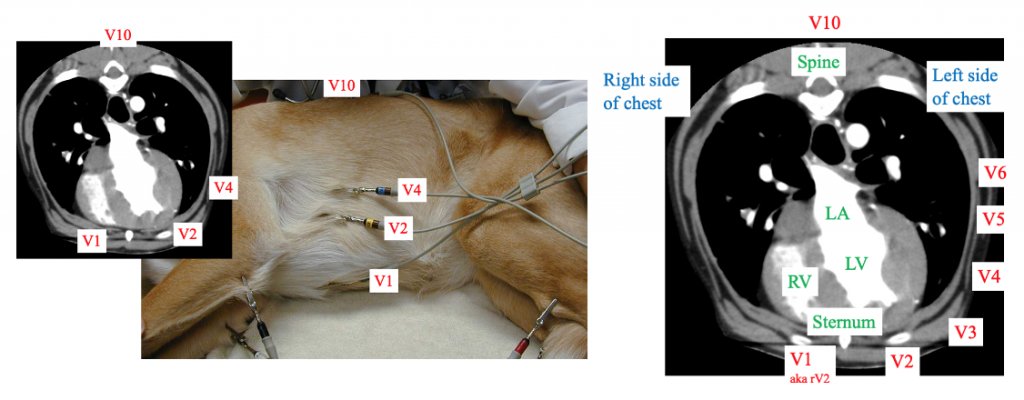
2. On occasion precordial electrocardiography may provide significant additional data; complementing and/or extending information obtained from limb leads
Detection of ventricular enlargement (increased sensitivity)


