Large Animal Cardiology
Created by V’22 cardio group revised from Dr. Suzanne Cunningham
Last Updated 12/2/20
History and Exam
History and Observation
- Information that may indicate a cardiovascular problem
- Reduced performance: more often will be attributed to musculoskeletal or respiratory issue
- Cough
- Dyspnea
- Stunted growth
- Lethargy
- Collapse
- Observe from a distance prior to physical exam. Note the following –
- Animal’s disposition
- Alert, dull, nervous, or quiet
- Dyspnea present?
- Any peripheral edema?
- Jugular pulsation or distension?
- Some degree of pulsation = normal in large animals
- If animal lowers head to graze → head is lower than right atrium → distension of entire jugular occurs
- This is NOT pathologic
- To determine pathologic distension: observe jugular vein when animal’s head is in normal position
- Pathologic = jugular vein pulsating beyond lower 1/3 of the neck → jugular distension. Consider pericardial or cardiac disease
Cardiovascular Exam
- Mucous membrane color and capillary refill time (CRT)
- Normal = moist, pink, CRT < 2 seconds
- Peripheral pulse
- Facial artery: rostroventral border of the mandible
- Transverse facial artery: caudal to the lateral canthus of the eye, ventral to the zygomatic arch
- Brachial artery: high on the medial aspect of the forelimb (also used for pulse detection)
- Cardiac apex beat palpate thorax wall with flat of hand. Useful in detecting thrills
- Thrill: a palpable vibration caused by turbulent blood flow. Present in murmurs graded V-VI/VI
- Auscultation of all regions of heart on left and right side of thorax
Cardiac Auscultation
- Entire precordium should be auscultated during exam
- Point of maximum intensity (PMI) of valves
- Mitral valve: left 5th ICS, dorsal to olecranon (cardiac apex)
- Aortic valve: left 3rd ICS, below point of shoulder and medial to triceps muscle mass (heart base)
- Pulmonic valve: slightly cranioventral to aortic valve at left heart base
- Tricuspid valve: right 3rd – 4th ICS medial to triceps just above olecranon
Valve locations for auscultation (P = pulmonic, A = aortic, M = Mitral, T = Tricuspid)
- Heart rate and rhythm assessment
- Horse: 44 BPM (23-48 range)
- Cow: 30 BPM (60-80 range)
- Sheep: 75 BPM (60-120 range)
- Goat: 90 BPM (70-120 range)
- Swine: 68 BPM (58-86 range)
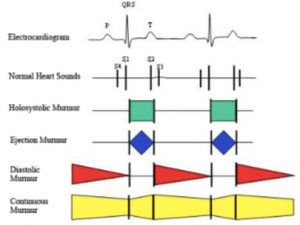
- It is normal to hear 2, 3, or 4 heart sounds in horse & cow!
- S1 = closure of mitral and tricuspid valve
- Systole occurs between S1 & S2
- S2 = closure of aortic and pulmonic valve
- S3 = vibrations resulting from termination of rapid ventricular filling in early diastole
- S4 = late diastole, during atrial contraction
- S1 = closure of mitral and tricuspid valve
Diagnostic Procedures
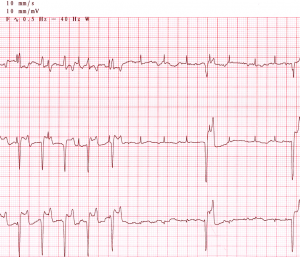
Electrocardiography (ECG)
- Use in large animals is limited to determination of heart rate and rhythm
- CANNOT get accurate information about chamber enlargement or mean electrical axis because of the “category B” distribution pattern of Purkinje fibers in ventricles of horse/cow – depolarization happens in single “burst” of activation, so multiple lead tracings are not accurate
- Can use single lead system (base-apex lead)
- Right forelimb (white) electrode → along jugular groove on right side of neck
- Ground (green) electrode → right base of neck
- Left limb (black and red) electrodes → over left precordium behind olecranon (left apex)
Echocardiography
- Non-invasive diagnostic technique allowing for real-time evaluation of blood flow and movement of walls/valves of heart
- Can measure wall thickness and luminal dimensions
- Best non-invasive diagnostic test for congenital and acquired heart disease
- When is an echo indicated?
- New/loud murmur
- Arrhythmia detected
- To rule out CHF
- Impaired athletic performance after musculoskeletal and respiratory disease are excluded
- Fever of unknown origin
Radiography
- Most helpful in foals: lateral AND dorsoventral views possible
- Angiography to identify congenital lesions
- Provides limited information from large adult horses
- Can only obtain lateral views
- Cardiac enlargement must be significant to detect
- +/- information about pulmonary infiltrates to aid in diagnosis of CHF
Bloodwork
- CBC: helpful to look for signs of infectious disease
- Endocarditis
- Bacterial pericarditis
- Serum chemistry: electrolytes, liver and kidney values, etc.
- Arterial blood gas: information about oxygenation and intracardiac shunts
- Serum cardiac Troponin I (cTnI): evaluate myocardial damage
Blood Pressure
- Dinamap indirect BP measurement on coccygeal artery (OR metatarsal in foals)
- Direct BP measurement = gold standard
- Requires arterial catheterization
- Useful for monitoring patient on cardioactive drug (i.e. Hydralazine – arterial vasodilator)
Cardiac Catheterization
- Not common in large animals
- Useful for critical care patients or diagnostic challenges
- Can demonstrate…
- Cardiac output
- Pulmonary hypertension
- Pressure profiles
- Oxygen contents of different cardiac chambers
- Pacemakers sometimes needed in donkeys & horses with symptomatic high-grade AV block
Cardiac Murmurs
- Clinical causes include
- Valvular disease
- Stenosis
- Insufficiencies
- Intra- or extra-cardiac shunts
- Septal defects
- PDA
- Sinus of Valsalva rupture
- Conditions à increased cardiac output
- Conditions à increased velocity of blood flow
- Anemia
- Fever
- High adrenergic tone
- Diastole = longest phase of cardiac cycle, therefore, longer murmurs are more likely to be diastolic
- Diastolic murmurs = MUCH more common in horses than small animals
- Aortic insufficiency = common finding in older horses
- Diastolic murmurs = MUCH more common in horses than small animals
- Valvular disease
Murmur Description
Grade I: Soft murmur, heard while listening in a quiet room/stall after listening for a prolonged period of time
Grade II: Soft murmur that can be heard almost immediately
Grade III: Low – moderate intensity murmur
Grade IV: Moderately intense murmur without a palpable thrill
Grade V: Loud murmur with the presence of a palpable precordial thrill
Grade VI: Loud murmur, palpable thrill. The murmur is audible with the stethoscope removed from the thorax
Congenital Murmurs
- Clinical signs of congenital defects = dependent upon severity of hemodynamic derangement
- Asymptomatic, reduced exercise tolerance à cyanosis and death
- VSD = most common defect seen in foal & calf
- Valvular defects = next in frequency
- Ventricular Septal Defect (VSD)
- Most common cardiac defect in horse/cattle
- Harsh, holosystolic murmur overriding S2; PMI = right side, +/- additional murmur over pulmonic region (= relative pulmonic stenosis)
- Cardiac cath – elevated RV pressures and PO2
- Echo – may visualize defect; agitated saline injection may show bubbles in BOTH R & L ventricles (bubble study)
- Patent Ductus Arteriosus (PDA)
- Continuous, machinery murmur; PMI = L base of heart, murmur radiates to manubrium of sternum & R cardiac base
- Uncommon to auscult continuous murmur in foal (systolic murmur = more common). If a murmur does NOT disappear by day 4 of life = pathologic/abnormal murmur
- Tetralogy of Fallot
- Systolic murmur transmitted widely over R & L thoracic wall
- Radiographs – RVE
- Cardiac cath – elevated RV pressure, lower pulmonary arterial pressure
- Stunting of growth, cyanosis, dyspnea
- defects
- Persistent truncus arteriosus
- Atrial septal defects
- Atrioventricular septal defects
- Valvular dysplasia or stenosis
- Other complex congenital lesions
Acquired Murmurs (valvular disease)
- Most valvular lesions do not halt athletic horses, however, it’s possible performance may decrease over time
- Exception: ruptured chordae tendinae → profound effect on performance
- Survival prognosis = good
- Functional (physiologic) murmur
- Benign, typically high frequency, low intensity, grade I-II/VI at rest (intensity can increase > III/VI if horse is excited or w/ colic)
- Usually crescendo-decrescendo; PMI = pulmonic/aortic valve (heart base)
- Common in young/athletic horses
- Functional murmurs disappear at rest
- Aortic Stenosis (AS)
- Crescendo-decrescendo (ejection quality) systolic murmur; PMI = Ao valve region
- Most outflow tract murmur in horse = Ao valve > pulmonic valve
- MOST likely of clinical significance if…
- Grade III/VI or louder
- Heard on both sides of chest
- Acquired AS is more common than congenital (subaortic) AS in horses
- Mitral insufficiency/regurgitation (MR)
- Holosystolic, plateau murmur; PMI = mitral area, may radiate towards aortic valve
- Second most common acquired valvular disease in horses, cattle, pigs
- Severe MR can → LCHF w/ coughing, exercise intolerance, dyspnea
- Mild MR may not be associated w/ clinical signs
- Acutely ruptured chordae tendinae → CV collapse w/ fulminant pulmonary edema
- Ruptured chordae tendinae
- Results in marked prolapse of MV leaflets w/ severe regurgitation
- Widely radiating pansystolic murmur
- Increased LA pressure → more pronounced/prolonged S3
- +/- Acute dyspnea, frothy nasal discharge due to pulmonary edema
- Tricuspid Insufficiency
- Harsh, holosystolic plateau murmur; PMI = right AV valve
- Most common acquired murmur in cattle, pigs, sheep (secondary to endocarditis)
- TR occasionally produces murmur in horse (common in standardbred racehorses)
- +/- Prominent jugular pulsations
- May be associated w/ high altitude disease in cattle or other causes of PHT
- Aortic Insufficiency
- Long diastolic decrescendo murmur; PMI = left hemothorax. Musical sounding
- The most common acquired valvular defect in aged horses
- Severe AI may → bounding, “waterhammer” arterial pulses due to diastolic runoff
- Echo: guarded – poor prognosis if…
- Fractional shortening < 30%
- LA > 16 cm diameter
- Pulmonary artery > aorta
- Pulmonic insufficiency and stenosis: rare in large animals
Cardiac Arrhythmias
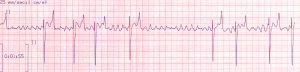
NORMAL Equine ECG
- Heart rate = 30 – 45 BPM at rest
- P Wave: bifid in lead II (can be single/polyphasic, too). Maximum amplitude ~ 0.5 mV. Duration 0.08 – 0.2 seconds
- PR Interval: duration 0.22 – 0.56 seconds
- QRS Complex: lower amplitude and more variation than in the dog. Not enough definitive diagnostic criteria to diagnose ventricular enlargement patterns
- T Wave: usually positive (leads III & aVF) or biphasic (lead II, aVR, aVF). Changes in T waves in normal horses with exercise or excitement
- T wave changes & ST segment changes: hypoxia, shock, septicemia, toxemia
Normal VARIATIONS in Equine ECG
- Sinus Arrhythmia and Wandering Pacemaker: occur in <30% normal horses at rest. Associated with high vagal tone, disappear with exercise or atropine. Not associated with respiration (like in dog)
- Low grade AV block: 1st degree AV block (PR interval > 0.40 sec) & Mobitz Type I (Wenckebach) 2nddegree AV block occurs in <20% of normal resting horses
- Are considered normal and due to high vagal tone if there are NO associated clinical signs and the rhythm returns to sinus rhythm with exercise, excitement, or atropine
- High-grade AV block or AV block that persists with exercise = pathologic. Dropping of every other beat/ 2+ beats in succession is NOT normal
- Sinus arrest and Sinoatrial Block: occasional pauses or breaks in normal sinus rhythm (NSR). Pauses usually disappear with exercise or atropine and do NOT require therapy
- Prolonged sinus arrest can → syncope, sometimes necessitating pacemaker placement
ABNORMAL Rhythms
- Atrial Fibrillation: common in horses, develops in two different populations of horses: (1) young horses of racing age without evidence of other cardiovascular disease, and (2) older horses with loud murmurs and significant cardiac pathology found upon necropsy
-
- Idiopathic atrial fibrillation: young horses, racing age. Present with sudden (an unexplained) loss of stamina
- Slow and irregular heart rate – may be confused with 2nd degree AV block or sinus arrest on auscultation
- Absent – soft murmur, usually without signs of heart failure early on
- Good prognosis for return to NSR with treatment
- Atrial fibrillation with concurrent heart disease: older horses, usually with loud murmurs of MR or TR
- Often evidence of heart failure
- Heart rate tends to be fast (70 – 100 BPM)
- May present for exercise intolerance, dyspnea, edema, weakness, or collapse
- Diagnosis: based on physical exam, detection of an irregular heartbeat & pulse. Confirmed by ECG. Evaluate for presence of underlying heart disease via echo
- Treatment
- When heart disease is absent – mild: conversion of atrial fibrillation to NSR via Quinidine
- Decreases automaticity, slows conduction, prolongs effective refractory period of atrial cells
- Negative inotrope with anti-vagal effects (like atropine)
- Well absorbed via PO administration through a nasogastric tube
- New techniques of transvenous cardioversion of atrial fibrillation in horses are beginning to replace oral cardioversion with Quinidine
- Possible SE: tachycardia, depression, urticaria, edema of nasal mucosa, anorexia, colic, diarrhea, laminitis, seizures, ventricular arrhythmias
- ONLY give Quinidine if animal has no systemic illness or CHF present
- When heart disease is absent – mild: conversion of atrial fibrillation to NSR via Quinidine
- Idiopathic atrial fibrillation: young horses, racing age. Present with sudden (an unexplained) loss of stamina
-
-
- When heart disease is present: initiate treatment to relieve signs of CHF and control the ventricular response rate to the fibrillating atria
- Administer Furosemide IV or IM (0.5 – 1.0 mg/kg) to control edema
- Maintenance Digoxin BID
- When heart disease is present: initiate treatment to relieve signs of CHF and control the ventricular response rate to the fibrillating atria
- Prognosis: fair – good when onset is recent and loud murmurs/signs of CHF are absent
- 75 – 85% of horses with atrial fibrillation will convert to NSR
- 20 – 30% of converted cases may revert back to atrial fibrillation
- Prognosis is dependent upon underlying heart disease
- The longer a horse has been in atrial fibrillation, the greater chance of recurrence (even after cardioversion)
-
- Atrial and ventricular arrhythmias
- If consistent or frequent – signs of heart disease (i.e. myocarditis). Can also be associated with…
- Septicemia
- Toxemia
- Acute GI disease
- Viral or bacterial diseases specific to horses
- Disease associations in horses
- Atrial tachycardia develops with myocardial disease
- Ventricular tachycardia develops with septicemia, toxemia, GI disturbances (non-cardiac causes)
- If consistent or frequent – signs of heart disease (i.e. myocarditis). Can also be associated with…
- Atrial Tachycardias
- Usually managed by digitalization supplemented with Quinidine in refractory cases
- Lidocaine: causes convulsions in horses so ONLY used at very low doses (0.25-0.5 mg/kg slow IV) if necessary, for ventricular tachycardia (VT)
- Ensure serum potassium levels are normal prior to administration
- Hypokalemia decreases the effectiveness of lidocaine
- Magnesium is used to treat quinidine induced torsades de pointes and also refractory ventricular tachycardia
Ventricular tachycardia to third degree AVB in a donkey
- Heart block in Horses
- Advanced (high grade) 2nd or 3rd degree block = occasional cause of syncope in horses
- High grade AV block is more common in donkeys/mules (syncope is often mistaken for seizures)
Third degree AV block in a donkey, lead II
Congenital Heart Defects – EQUINE
Ventricular Septal Defect
- Varies in size, often located in the upper, membranous septum
- Is NOT typically accompanied by another congenital defect (different than bovine VSD)
- Clinical signs are dependent on the severity of the defect
- Stunted growth
- Exercise intolerance
- Heart failure
- +/- Normal longevity (small defects)
- Physical findings
- Harsh, holosystolic murmur. Usually accompanied by a thrill
- PMI = Right 2-4 ICS, radiates
- +/- Signs of LV failure
- A high, large VSD can undermine the support of the aortic valve → Aortic Regurgitation → diastolic murmur in addition to the systolic murmur of the VSD
- ECG: normal or suggestive of LVE
- Radiographs
- Variable, often WNL
- +/- Generalized cardiac enlargement
- +/- Enlarged MPA
- +/- Vascular pattern from pulmonary overcirculation associated with left-to-right shunting
- Cardiac Catheterization
- Significant shunting
- Oxygen saturation of the pulmonary artery blood >>>> oxygen saturation of the RA blood
- Severe cases: RV and pulmonary artery pressures elevated (reactive PHT)
Tetralogy of Fallot
- Clinical presentation
- Stunting of growth
- Cyanosis
- Dyspnea
- Exercise intolerance
- Physical findings
- Systolic murmur radiating widely over cardiac area
- ECG: RVE
- Radiographs: RVE
- Cardiac catheterization
- Elevated RV pressure
- Normal – low pulmonary artery pressure
- Low aortic blood oxygenation
Patent Ductus Arteriosus
- Foals: grade II-III/VI continuous murmur, PMI = 3rd – 4th left ICS at level of point of shoulder
- Heard until 4 – 5 days post birth
Other defects
- Complex cardiac defects reported in Arabian foals
- Atrial septal defect
- Endocardial cushion defects
Congenital Heart Defects – BOVINE
Ventricular Septal Defect
- Often coexists with another heart defect (i.e. truncus arteriosus) – unlike horses
- Two-dimensional and Doppler echo = diagnostic
- Cardiac cath is rarely performed
Other defects
- Ectopia cordis: the heart is located most often in the neck
- PDA: usually diagnosed based on characteristic murmur
Acquired Cardiac Diseases
Aortic Valve Insufficiency in the Horse
- Pathology
- Diffusely thickened aortic valve OR nodules/bands affecting valve
- Nodules = most common, loose fibrous connective tissue, fibroblast abundant
- Clinical Signs
- Diastolic decrescendo murmur, PMI = L heart base
- +/- Bounding pulses
- CHF & cardiomegaly in older animals (after peak working years)
- Diagnosis
- Based on physical exam
- ECG suggestive of L heart enlargement
- Echo to document aortic insufficiency
- Presence of fever/leukocytosis/peripheral embolization → consider bacterial endocarditis
- Treatment
- Most affected horses are NOT symptomatic, are old and not being worked
- No adequate therapy
- If CHF – Digitalis and diuretics
- Aortic valve more commonly affected than mitral valve
Mitral Valve Insufficiency in the Horse
- Pathology
- Localized or diffuse thickening, nodular thickening OR combination of lesions
- Diffuse fibrous thickening = most common
- Clinical Signs
- Most affected horses are asymptomatic
- Middle – older age: can be severe enough to → exercise intolerance +/- CHF
- Grade III+/VI plateau-shaped holosystolic murmur, PMI = mitral area, radiating to right side
- Diagnosis
- Based on physical exam
- Echo to support: L heart volume overload in absence of AI
- Normal Thoroughbreds: small amount of MR/TR present, especially after training
- Mitral valve prolapse can occur with MR (less severe than degenerative valvular disease)
- Prognosis
- Good: mitral insufficiency rarely → CHF in horse
- If progression to CHF occurs = poor prognosis
- Poor oral absorption of diuretics & ACE-inhibitors
Ruptured Chordae Tendinae in the Horse
- Chordae tendinae: anchor valve cusps to papillary muscles
- Rupture → grossly incompetent valve
- Large volume of blood regurgitated into LA during systole → decreased CO, increased LVEDV & LVEDP → pulmonary congestion & fulminant life-threatening edema = LCHF
- +/- Sudden death
- Causes of ruptured MV chordae
- Blunt trauma
- Severe physical exertion
- Underlying primary MVD
- Clinical signs
- Acute dyspnea with white foamy discharge from nostrils
- Loud pansystolic murmur, PMI = MV, usually with palpable thrill
- Decreased CO → signs of low output heart failure or CV collapse
- Diagnosis
- Echo to visualize severe MR and a flail MV leaflet
- Radiographs may show pulmonary infiltrates from LCHF
- Prognosis
- Grave: most animals will be euthanized for fulminant CHF
Aorto-Cardiac Fistula (Ruptured Sinus of Valsalva) in the Horse
- Acquired cardiac fistula
- Middle-aged, breeding stallions
- Occurs suddenly → rapid death or severe distress
- Clinical signs
- Acute collapse
- Respiratory distress
- Severe exercise intolerance
- Continuous (PDA-like) murmur, PMI = R 4th ICS
- Diagnosis
- Rupture should be suspected in breeding stallions with characteristic continuous murmur and appropriate clinical signs
- Echo to confirm diagnosis: visualize fistula from R aortic sinus with continuous left → right shunting from LVOT → RV or RA
- ECG may show unifocal ventricular tachycardia
- Treatment
- Supportive therapy – complete rest
- Furosemide
- Ventricular antiarrhythmics or digoxin
- Prognosis
- Usually grave: survival time = 24 hr. – 4 yr. (if able to stabilize)
- Sudden death possible
Bacterial Endocarditis in Ruminants
- Degenerative valvular disease = uncommon in ruminants
- In ruminants: bacterial endocarditis appears as vegetative lesions, mostly on the right side of circulation – Tricuspid and Pulmonic valves
- Pathogenic Organisms (vary w/ species)
- Horse: Streptococcus, Actinobacillus, Pasturella
- Cattle & Goats: Arcanobacterium pyogenes, Streptococci
- Swine: Erysipelothrix rhysiopathiae, Streptococci
- Lambs: Enterococci
- Clinical Signs
- Recurrent fever
- Anorexia
- Weight loss
- Poor milk production
- Shifting leg lameness
- Tachycardia
- Tachypnea
- History of traumatic reticuloperitonitis or pneumonia
- 1/6 cases admitted with primary complaint of heart disease
- Physical Examination: nonspecific and non-localizing
- Systolic murmur may be present over TV and PV
- Diastolic murmur of PI may be present
- Jugular distension & jugular pulses together with distension of mammary veins may be observed → development of ventral edema, ascites, cachexia
- Diagnosis
- History, physical signs (murmur, fever), positive blood cultures
- Echo visualization of vegetative lesions
- Leukocytosis
- Neutrophilia
- Lymphopenia
- Hyperglobulinemia
- Anemia due to chronic infection
- Treatment
- High dose antibiotics 4-6 wk. (penicillin or ampicillin) unless c/s indicate otherwise
- Prognosis
- Varies with stage of disease
- Early (no heart failure): fair
- Heart failure present: guarded – poor
- Varies with stage of disease
Myocardial Disease in the Horse
- Primary myocardial disease = cardiomyopathy, not well documented in horses
- Myocardial failure in the horse = most commonly from ingestion of monensin
- Myocarditis (w/o CHF) = most frequently recognized myocardial disease in the horse
- Myocarditis
- Inflammatory or degenerative myocardial lesions found in 2-15% necropsied horses
- Bacterial, viral, or parasitic causes (Streptococcus equi, influenza, purpura hemorrhagica, equine infectious anemia, strongyle larvae)
- Strongyle larvae damage aortic root → microemboli → arteriosclerosis & myocardial necrosis
- Other causes: endocarditis, thoracic/abdominal abscessation, guttural pouch infections, colic, toxemias
- EHV-1 → myocarditis = well documented in aborted equine fetuses
- Clinical signs = often absent
- Decreased performance
- Dyspnea on exertion
- Tachycardia disproportionate to fever
- Arrhythmias
- Murmurs
- Loud gallop sounds
- Fainting/collapse
- Sudden death: reported in horses recently recovered from strangles/influenza
- Development of CHF
- Treatment: directed at primary illness (cause of myocarditis)
- Stall rest for 4 – 6 mo.
- Antiarrhythmic therapy if serious arrhythmia is detected
- Digitalis & diuretics if CHF present
- Monensin toxicosis
- Horses = more sensitive to monensin than cattle, develop cardiac signs if ingest treated cattle feed
- Clinical signs
- Acutely affected
- Abdominal pain
- Diarrhea
- Acute circulatory failure
- Death
- Delayed syndrome: 3 – 6 mo. post-ingestion
- Necropsy
- Myocardial degeneration
- Pericardial effusion
- Evidence of heart failure
- Treatment: supportive, myocardial damage is irreversible
- Acutely affected
- White snakeroot intoxication
- Ingestion → severe myocardial degeneration, hemorrhages, infarcts
- Arrhythmias & sudden death = frequent sequelae
Myocardial Disease in Cattle
- Cardiomyopathy is rare in cattle
- Bovine DCM reported in some breeds
- Myocardial disease in cattle is typically secondary to…
- Systemic infection
- Pneumonia
- Traumatic reticulopericarditis
- Neonatal infection
- Mastitis
- Nutritional deficiency
- Vitamin E
- Selenium
- Neoplastic infiltration
- Lymphosarcoma
- Ingestion of toxins
- Monensin
- Gossypol
- White snakeroot
- Cassia occidentalis
- Clinical syndromes will vary (sudden death – chronic CHF)
- Systemic infection
Traumatic Pericarditis in Cattle
- Most common cause of CHF in cattle
- Perforation or migration of a foreign body (i.e. wire) into the pericardial sac. Disease course varies from few d. – few wk./mo.
- Pathology
- Significantly thickened pericardial sac
- Adhesions between pericardium & diaphragm and pericardium & epicardium
- +/- Visualize foreign body
- Variable amounts of pus, fibrin, gas
- Clinical signs: signs reflect presence of infection due to reticuloperitonitis with evidence of cardiac tamponade
- Depression, anorexia, weight loss
- Diarrhea, constipation, rumen atony
- Decreased milk production
- Arched back, abducted elbows, pain
- Fever, tachycardia, tachypnea
- Venous distension of the jugular and mammary veins
- Ventral and cervical edema, ascites later in disease course
- Physical findings
- Early in disease: pericardial friction rub may be present
- Later in disease
- Pericardial effusion develops → muffled heart sounds
- Gas and fluid accumulate → splashing, tinkling, gurgling sounds synchronous with heartbeat
- Diagnosis
- Rule outs
- Heart failure from congenital defects
- Infective endocarditis
- Altitude sickness (PHT)
- Lymphosarcoma
- Other myocardial diseases
- To confirm diagnosis
- Echo
- Pericardiocentesis at 4th – 5th ICS on Left side (idiopathic effusions can occur and will often resolve)
- Treatment
- Drain pericardial sac when heart failure is present
- Pericardiocentesis
- Instillation of antibiotics, debriding enzymes, placement of pericardial drain/surgical exposure and drainage
- Prognosis = poor
- Drain pericardial sac when heart failure is present
- Rule outs
Pericardial Disease in the Horse
- An “epidemic” of pericarditis and mare reproductive loss in Spring-Summer of 2001 in Kentucky (previously very rare). Actinobacillus were the principal isolates
- Cause of outbreak: “Septic penetrating setal emboli (SPSE)” from infestation of eastern tent caterpillars
- Clinical signs
- Fever, anorexia, lethargy
- Muffled heart sounds +/- pericardial friction rub
- Signs of RCHF
- Jugular distension
- Jugular pulses
- Ventral edema
- Ascites
- Pleural effusion
- Tachycardia
- Diagnosis
- Rule out other causes of RCHF
- Rule out pleural effusion due to pleuritis
- Echo or successful pericardiocentesis to confirm diagnosis
- Can measure RA pressure before and after pericardiocentesis
- +/- Low voltage QRS complexes or electrical alternans on ECG (not as helpful in diagnosing as in small animals)
- Treatment
- Signs of systemic congestion: drain and lavage pericardial sac
- Systemic antibiotics, sometimes even if negative culture
- If large number of eosinophils OR if infectious etiology is excluded → consider corticosteroid therapy
Neoplasia
- Lymphosarcoma = most common neoplasia of the heart in cattle
- Consider as a differential diagnosis for most cardiac diseases in cattle
- Less frequent in horse – if it occurs, may include heart