CARDIOLOGY PHYSICAL EXAMINATION
Created by V’22 cardio group modified from Dr. John Rush
Updated 03/26/2020
As with any clinical exam, the cardiology physical exam starts by obtaining a patient history from the owner and hands-off observation of the animal.
Tips Before the Physical Exam:
1. Be careful how you phrase questions. Ask specific, open-ended questions to collect as much information as possible from the client
2. Key questions to ask: when clinical signs began, frequency and duration of the sign, timing (nocturnal dyspnea for example), activity level, respiratory signs (with a description of the cough consistency, if there is one), diet, and prior medical history
3. General observation should include assessment of body condition, overall health, ambulation, and respiratory effort
4. Some animals can be asymptomatic in early heart disease due to compensatory mechanisms of the body to increase preload, cardiac filling, and stroke volume. These compensatory mechanisms, over time, can get overwhelmed and lead to heart failure and damage to other organs
Common Clinical Manifestations of Heart Disease:
1. General weakness and lethargy
2. Exercise intolerance: A common sign in dogs with reduced cardiac output
3. Respiratory signs such as dyspnea (nocturnal, especially), tachypnea, panting, coughing, and orthopnea
a. Respiratory signs can be related to cardiogenic sources but also can be purely related to respiratory illness, so it is important to discover the underlying cause to best treat the condition. Cardiovascular and respiratory diseases can often occur together
b. Nocturnal dyspnea is characteristic of left-sided congestive heart failure
c. Dyspnea in heart disease usually starts as difficulty breathing with exertion but soon progresses to occur at rest. The animal commonly appears restless as it is trying to obtain dyspneic relief
d. A cardiogenic cough commonly presents as a husky, cough which may end with gagging and bloody foam. However, the character of the cough could change depending if the heart is enlarged and putting pressure on the airways
4. Cyanosis: blue color of skin and mucous membranes caused by the presence of reduced oxygenated hemoglobin in blood vessels. This can occur due to a reduction in the oxygen saturation of capillary blood
a. Central cyanosis: mucous membranes and skin (see photo 1)
b. Peripheral cyanosis: blood flow to a local area is restricted (as with thromboembolism)
5. Differential cyanosis: caudal mucous membranes (such as at the vulva or prepuce) are cyanotic but the cranial ones (lips and gums) are not. This is seen in right-to-left shunting PDAs

6. Abdominal distention and peripheral edema: this can occur as a consequence of right-sided congestive heart failure, along with hepatomegaly
7. Syncope: acute loss of consciousness due to interruption of blood flow to the brain
a. Recovery is usually rapid as the episode only lasts up to a few minutes. This is one way to distinguish syncope from a seizure, which typically has a post-ictal phase consisting of a change in behavior after the episode
8. Weight loss or cachexia
The Physical Exam: These steps can be performed in multiple different orders. What is important is that you find an approach or systematic fashion that works for you, so that you do not forget vital steps of the exam
1. Mucous Membranes
a. Check the cranial mucous membranes (lips and gums) for color and perfusion. Normal color is pink, whereas cyanosis (blue), pale (white), or hyperperfusion or injected membranes (bright red) indicate problems such as hypoxemia, poor perfusion, and inflammation/septic shock respectively
b. Test the capillary refill time of the membranes: press firmly on the gum briefly and release. Color should return within 2 seconds if perfusion is normal
c. Check for differential cyanosis as mentioned above. Check the membranes of the prepuce or vulva. You can also check for obstruction of blood flow to a certain part of the body, such as the limbs (best observed at the nail beds)
d. Keep in mind breed differences – i.e. Boxers and Great Danes naturally run more pink than most dogs, so it can be hard to distinguish their normal membrane color from situations that lead to injected membranes
2. Ocular Fundus Evaluation
a. This is a way to observe the arterial system directly
b. Severe heart disease can sometimes present as detached retinas and ocular hemorrhage, initially. This can sometimes be seen without specialized ocular equipment by observing dilated pupils (see photo 3)

3. Check the thyroid (especially cats)
a. Feline hyperthyroidism can sometimes present concurrently with heart disease
b. Start at the larynx and move your fingers slow and steadily downward to the thoracic inlet. You are feeling for the thyroid gland to “blip” below your fingers. You may be able to visually observe this in cats with very large glands, but this test is based primarily on feel
4. Jugular veins
a. We are looking for inappropriate distention or pulsation related to right-sided cardiac events
b. Standing (or sternal recumbency) is preferred with the animal’s muzzle turned up 45 degrees and head turned 20 to 45 degrees to one direction
c. Observe the jugular vein at the level of the thoracic inlet and above by the jugular furrow (usually the air does not need to be clipped, and the hairs may accentuate the vein motion)
-The normal jugular vein can be seen pulsating slightly at the level of the inlet in rhythm with the cardiac cycle. It should not pulsate above the bottom 1/3 of the neck (see photo 4)
-If the jugular vein has large pulsations, or if the vein is distended higher up the neck (especially if more than ½ way up the neck), this may be a sign of right-sided congestive heart failure.
d. Having trouble seeing the vein? Apply pressure to occlude the vein at the inlet, then watch and feel for the vein. When pressure is removed, the blood should drain in less than half a second and the vein should no longer appear distended
-Delay in drainage indicates that the right heart cannot deal with a small bolus of blood and may indicate imminent right sided heart failure
e. The right side of the heart tends to fill more with inspiration, so the vein may be more distended with inspiration
f. Make sure the jugular veins are symmetrical. If one jugular palpates as a firm cord, there could be thrombosis present

5. Palpation of the thorax/chest wall/apical impulse
a. Feel for the apex beat near the left 5th intercostal space below the costochondral junction. You will feel this better in skinny, deep chested dogs
-With enlargement, the apex beat can shift caudally
-Patients with shock or severe hypovolemia may have a diminished apex beat
-In addition to cardiac enlargement, displacement of the apex beat can alternatively indicate a space occupying mass or collapse of a lung, shifting the heart’s location
b. Palpate the arterial pulse or the apex beat of the heart while simultaneously visualizing the jugular vein to get a better understanding of the overall cardiac cycle
c. Palpate for right ventricular activity on the right side in the tricuspid area, or the 4th intercostal space above the costochondral junction. The apex beat should be stronger on the left than the right side of the chest
d. With experience, you can get an impression of cardiac hypertrophy (or high sympathetic tone) just by feeling a lifting sensation where the heart contacts the thorax
e. Using the flat of your hand pressed against the thorax, feel for a thrill
-A palpable thrill is a vibrating sensation that is present in heart murmurs grade V/VI or VI/VI, representing the palpable manifestation of turbulent blood flow
6. Palpation of the abdomen/caudal body
a. Hepatojugular reflux: with the animal in standing position, compress the cranial abdomen upward and forward to temporarily increase venous return. Do this while observing the jugular veins (see photo 5)
-A compliant right heart would accept this bolus by distending with minimal increase in pressure. There should be no more than a transient distention of the jugular vein
-A persistent elevation of the jugular vein during this maneuver means that the right heart cannot accommodate the extra blood, and right heart failure may be imminent
-You can also auscultate at the left ventricular apex while doing this to bring out a gallop rhythm
b. Feel for general abdominal organomegaly due to hepatic or splenic enlargement
c. Check for abdominal effusion by keeping one hand on the side of the abdomen and tapping the opposite side briskly
-You are attempting to sense a fluid wave

Photo 5. An example of the hepatojugular reflux. The cranial abdomen is pushed up and inward to increase venous return to the right side of the heart while also observing the jugular veins. If the right heart cannot accommodate this change in fluid balance, then the jugular vein will be persistently distended during compression, and right-sided heart failure could develop.
7. Palpation of pulses
a. To feel the femoral pulses, palpate proximally in the groin area (see photo 6)
-Pulse pressure is the variation between systolic and diastolic pressure. Your fingers are sensitive to this, but not to the absolute blood pressure
-Your fingers get used to feeling a 40 mm Hg difference (e.g., the difference felt in a dog with a blood pressure of 120/80 mm Hg). Wider pulse pressures feel like bounding pulses (e.g., 120/50 mm Hg). Narrow pulse differences feel like weak arterial pulses (e.g., 120/95 mm Hg).
b. Evaluate the pulse rate, rhythm, and character
-Record if pulses are weak, bounding, or out of sync with the heart
-Feel pulses and auscultate at the same time to pick up pulse deficits. A heartbeat heard without a corresponding arterial pulse is a pulse deficit

8. Auscultation of the thorax
a. Listen to the heart and lungs when the animal is standing
-Avoid artifact: it may be necessary to intermittedly hold the muzzle of a panting dog or trick a purring cat with running water or alcohol-soaked cotton balls
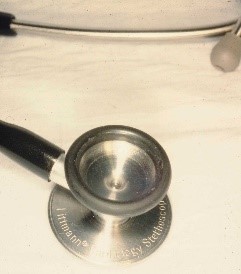
b. Listen over all of the valves of the heart (see photo 7)
-Left side: Pulmonic valve (approximately 3rd intercostal), aortic valve (approximately 4th intercostal), and mitral valve (approximately 5th intercostal).
-Use the mnemonic “PAM” to remember the order on the left side of the chest
-Right side: tricuspid valve; also usually the loudest location for a ventricular septal defect
-Heart sounds in cats are more audible parasternally, just to the right or left side of the sternum

c. You should always hear the S1 and S2 sounds. These are the “lub-dub” sounds
-S1 corresponds with the closure of the AV valves, heard best at the mitral valve near the cardiac apex
-S2 corresponds with the closure of the semilunar valves, heard best at the aortic valve at the heart base
-Systole is the period of time between S1 and S2
-Diastole is the period of time following S2 before the next S1. The length of diastole should be longer than systole in most relaxed animals
Murmurs
1. Questions to keep in mind: is the murmur systolic, diastolic, or both? Is it more intense on the left or right side? Is it more intense toward the apex of the heart or the base? (see photo 8)
2. Those originating from the right side of the heart tend to increase with inspiration and those from the left side increase with expiration
3. Some murmurs are defined as “crescendo-decrescendo”, which means that they are heard louder in the first half and softer in the second half of the cardiac systolic cycle

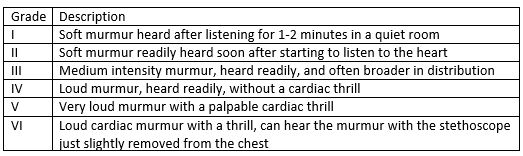
Grading of Murmurs
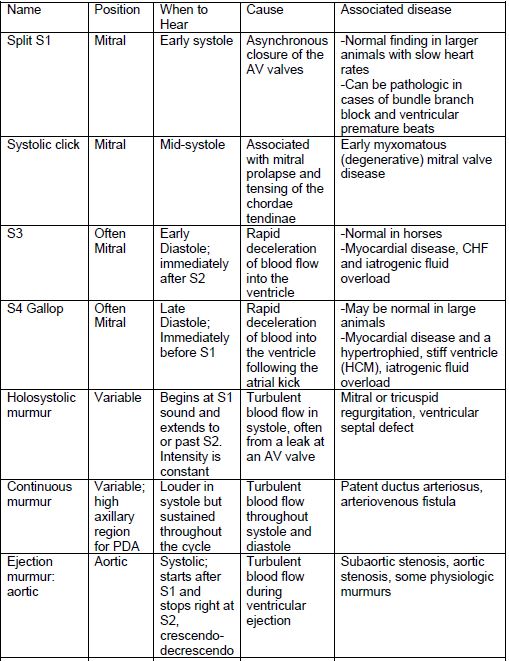
Abnormal Heart Sounds