Designed to improve the consistency and quality of individualized care for patients, RDs follow the Nutrition Care Process (NCP), established by the Academy of Nutrition and Dietetics (AND) that includes a Nutrition Assessment, Nutrition Diagnosis, Nutrition Intervention, and Nutrition Monitoring and Evaluation steps [1,2]. Specifically, Nutrition Monitoring and Evaluation is used to determine and measure the amount of progress made for the nutrition intervention and whether the nutrition related goals and expected outcomes are being met [3]. In order to assess such progress, RDs will frequently reference the patient’s EMR; however, access to such systems is not always possible in humanitarian crises despite their importance in disaster-related medical responses [4–6]. We provide these tools to improve the resilience and continuity of care of health services using easily-adapted, ready-to-use patient nutrition status screeners, trackers, and nutrition status assessments.
References
- AND Nutrition Care Process Available online: https://www.andeal.org/ncp (accessed on 3 May 2021).
- The Academy Quality Management Committee Academy of Nutrition and Dietetics: Revised 2017 Scope of Practice for the Registered Dietitian Nutritionist. Journal of the Academy of Nutrition and Dietetics 2017, 118, 141–165, doi:10.1016/j.jand.2017.10.002.
- AND NCP Step 4: Nutrition Monitoring and Evaluation 2018.
- Horahan, K.; Morchel, H.; Raheem, M.; Stevens, L.; Pawlak, S. Electronic Health Records Access during a Disaster. 1 2014, 5, doi:10.5210/ojphi.v5i3.4826.
- Oza, S.; Jazayeri, D.; Teich, J.M.; Ball, E.; Nankubuge, P.A.; Rwebembera, J.; Wing, K.; Sesay, A.A.; Kanter, A.S.; Ramos, G.D.; et al. Development and Deployment of the OpenMRS-Ebola Electronic Health Record System for an Ebola Treatment Center in Sierra Leone. J Med Internet Res 2017, 19, e294, doi:10.2196/jmir.7881.
- deRiel, E.; Puttkammer, N.; Hyppolite, N.; Diallo, J.; Wagner, S.; Honoré, J.G.; Balan, J.G.; Celestin, N.; Vallès, J.S.; Duval, N.; et al. Success Factors for Implementing and Sustaining a Mature Electronic Medical Record in a Low-Resource Setting: A Case Study of ISanté in Haiti. Health Policy and Planning 2017, 33, 237–246, doi:10.1093/heapol/czx171.
Purpose: The Nutrition Screening Form is designed to collect nutrition-related information on all inpatients as efficiently as possible. This form was adapted from the Mini Nutritional Assessment and Subjective Global Assessment screening tools [1-3]. Questions specifically target the patients’ ability to chew and swallow, food preferences, and food allergies to inform the composition and texture of therapeutic meals that patient receives.
Utilization: Prior to use, update the following fields:
- ‘eFIND#’ to the field hospital’s/emergency facility’s medical record numbering system
- ‘Pod #’ to the field hospital’s/emergency facility’s ward or floor division structure
This form can be used for initial and reassessment interviews by NTDRs to identify individuals at risk for malnutrition. A patient is classified as at risk for malnutrition and referred to a clinical dietitian if they report a ‘fair’ or ‘poor appetite’ appetite history and a ‘recent’ and ‘unintentional’ weight loss history. Patient-reported chewing or swallowing difficulties, cultural/religious food preferences, and food allergies should be communicated to food service staff. This information should also be updated on the Patient Census and Diet Order Tracker (see Tracker for patient census and diet orders below).
Download: A PDF fillable version of the Nutrition Screening Form can be found here!
Example of Nutrition Screening Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
References
- MNA Mini Nutritional Assessment (MNA) 2009.
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment Short-Form (MNA-SF): A Practical Tool for Identification of Nutritional Status. J Nutr Health Aging 2009, 13, 782–788, doi:10.1007/s12603-009-0214-7.
- Detsky, A.S.; McLaughlin; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What Is Subjective Global Assessment of Nutritional Status? Journal of Parenteral and Enteral Nutrition 1987, 11, 8–13, doi:https://doi.org/10.1177/014860718701100108.
Purpose: The Modified ADIME Note was adapted from Standardized Form 600: Chronological Record of Medical Care and the Nutrition Care Process note writing style [1–3]. ADIME stands for Assessment, Diagnosis, Intervention, Monitoring, and Evaluation – a five step process for examining the nutrition status of a patient. In the absence of an EMR, this reporting format prioritizes the assessment, diagnosis, and intervention components of ADIME, and enhances medical documentation efficiency.
Utilization: Prior to use, update the ‘eFIND#’ to the field hospital’s medical record numbering system. After providing individual MNT, clinical RDs should document their nutrition assessment, diagnosis, and intervention plan and recommendations using the Modified ADIME Note. This document should be placed into the patient’s medical record and steps should be taken to communicate nutrition recommendations with the patient’s primary care manager to optimize continuity of care.
Download: A PDF fillable version of the Modified ADIME Note Form can be found here!
Example of Modified ADIME Note Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
References
- US General Services Administration Standard Form 600: Chronological Record of Medical Care.
- Lacey, K.; Pritchett, E. Nutrition Care Process and Model: ADA Adopts Road Map to Quality Care and Outcomes Management. J Am Diet Assoc 2003, 103, 1061–1072, doi:10.1016/s0002-8223(03)00971-4.
- Thompson, K.L.; Davidson, P.; Swan, W.I.; Hand, R.K.; Rising, C.; Dunn, A.V.; Lewis, N.; Murphy, W.J. Nutrition Care Process Chains: The “Missing Link” between Research and Evidence-Based Practice. J Acad Nutr Diet 2015, 115, 1491–1498, doi:10.1016/j.jand.2015.04.014.
Purpose: The Patient Census and Diet Order Tracker is designed to facilitate meal forecasting in a disaster response setting. This is done by recording the number of patients consuming different types of meals over pre-determined mealtimes in a field hospital. Daily and weekly tallies of delivered meals can be used to estimate the popularity of food supplies in the patient population. This tracker also serves as a quality control tool in which the total number of meals delivered per food service period (e.g., breakfast, lunch, and dinner) can be matched to the current patient census.
Utilization: This tool is available as a weekly hard-copy tracker or as a modifiable Excel file. Prior to use, update the following fields:
- ‘Diet Orders’ to reflect the diet order types available at the field hospital; and
- ‘Date’ to ensure that the start date of each week is the day that meal forecasts must be distributed to the food suppliers.
This tracker carefully integrates with diet order and food allergy information to serve as a monitoring tool for successful and accurate meal delivery. This is done by recording the number of persons served for breakfast, lunch, and dinner according to each diet order. After each week, total meals served provides an estimate of the number of meals needed for the next week. This inventory assessment helps maintain adequate forecasting of supplies with food contractors. Additionally, this tool helps maintain proper food safety assurance and meal delivery coverage in accordance with USPHS Food Safety regulations.
Download: An Excel fillable calculator of the Patient Census and Diet Order Tracker can be found here!
Example of Patient Census and Diet Order Tracker used at the Javits New York Medical Station from 28 April through 01 May of 2020:
To best use this tracker, we recommend the following:
- One hour prior to meal delivery, personnel charged with delivering meals to patients should update the ‘Total Census' with the total number of patients in the hospital (Example A).
- The tracker should then be distributed to food service personnel responsible for producing and supplying meals to inpatients.
- Food service personnel should calculate the correct quantity and type of meals by multiplying the total patient census and the percentage of orders per diet order type. Food service personnel will then package, store, and deliver meals in accordance with standard processes.
- Within 30 minutes of meal delivery to patients, meal delivery personnel should:
- Tally diet orders per hospital ward to provide a total number of meals served by diet order type.
- Update the tracker with the total number of meals distributed to all patients.
- Compare the alignment of total 'Meals Served' to the 'Total Census’ (Example A).
- In the Excel version, ‘Meals Served’ auto calculates the sum of all meals delivered by diet order type to an aggregate total.
- Discrepancies between meals served and patient census totals should be addressed by food service personnel in the following ways:
- If fewer meals than the total census were served:
- Verify the current hospital census at the end of the meal period and identify if patients were discharged from the hospital during meal delivery.
- Verify diet ward rosters to ensure that all patients identified at the beginning of the meal period received a meal.
After delivering all meals, nutrition operations personnel should identify new hospital admissions during meal delivery and provide appropriate meal options in accordance with medical and nutritional prognoses.
- If more meals than the total census were served:
- Identify if and how many double-portion diet orders were placed by medical or nutritional staff.
- Provide a note indicating which patient(s) received double portions to properly adjust diet order tallies.
- Once all daily values are verified, report the sum of all ‘Meals Served’ and ‘Diet Orders’ in the ‘Weekly Totals’ column (Example B).
- In the Excel version, 'Weekly Totals' for 'Meals Served' and ‘Diet Orders’ will auto-populate.
- Distribute the completed tracker to food suppliers once data have been finalized on the seventh day of the weekly cycle.
- Calculate the ‘% of Meals Served’ per diet order by dividing the ‘Weekly Totals for Diet Order 1’ by the ‘Weekly Total of Meals Served’ and multiplying the output by 100.
- The sum of all the ‘% of Meals Served’ should total 100%
- Use the product of the '% of Meals Served’ and weekly total of each diet order to facilitate meal forecasting for the following weekly cycle.
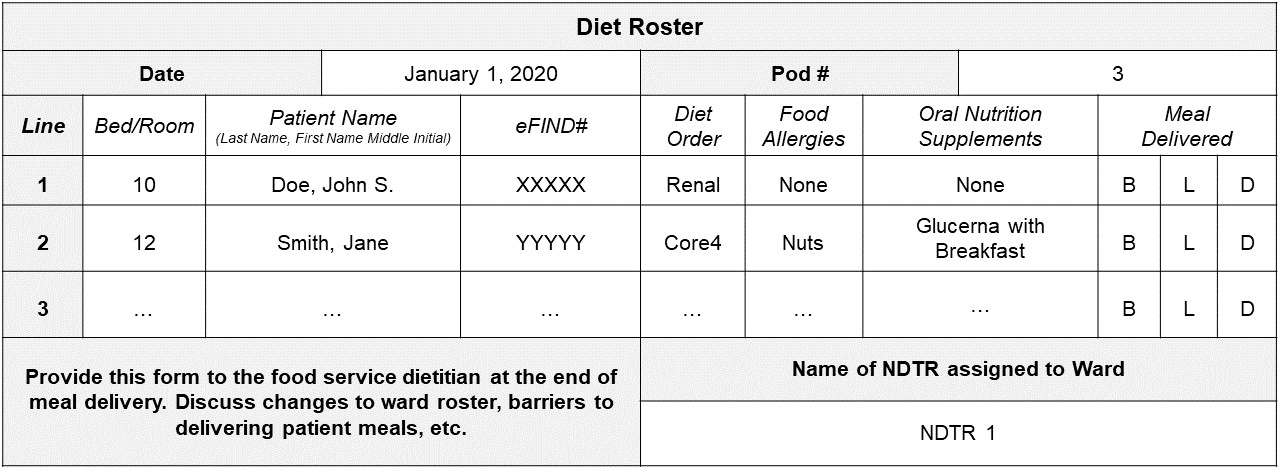
Purpose: The Diet Roster is designed to quickly identify patients’ diet orders, food allergies, and oral nutrition supplement requirements during meal delivery. The roster should be completed for every patient ward or floor by the assigned NDTR. This form should be reviewed and updated regularly as patients are admitted and discharged.
Utilization: First, update the ‘eFIND#’ to the field hospital’s medical record numbering system. Prior to meal delivery, NDTRs should review the patient’s medical record to verify their diet order, food allergy information, and oral nutrition supplement requirements. This information should be transcribed onto the diet roster. This form is then referenced when building patient meal delivery carts. After the patient meal is delivered, NDTRs cross off the appropriate ‘Meal Delivered’ column (‘B’ for breakfast, ‘L’ for lunch, and ‘D’ for dinner). After all patients on the assigned ward or floor have received a meal, the NDTR submits the roster to the food service dietitian. The food service dietitian then uses the roster to:
- Determine the number of meals delivered per meal period (to be used in the Patient Census and Diet Order Tracker shown above)
- Update the Patient Census and Diet Order Tracker with changes to diet orders or oral nutrition supplement requirements and food allergy information
Download: A PDF fillable version of the Diet Roster Form can be found here!
Example of Modified ADIME Note Form used at the Javits New York Medical Station from 28 April through 01 May of 2020: