The Nutrition Response Toolkit for Humanitarian Crises is designed to provide standardized, low-cost, easily adaptable crisis nutrition operational protocols for implementation in future field hospital deployments. In many humanitarian crises, field hospitals lack sufficient medical supplies and personnel to properly prepare, provide, and sustain food services and clinical nutrition assessments. Furthermore, nutrition personnel may lack the training or guidance on how to coordinate food services or conduct rapid clinical nutrition assessments. These challenges necessitate the creation of a standardized nutrition emergency response toolkit that can provide Registered Dietitians (RDs) and other nutrition personnel with:
1. Staffing models and training recommendations for field environments;
2. Record-keeping systems to monitor nutrition status, allergies, and dietary needs;
3. Food delivery trackers and meal forecasting calculators;
4. Therapeutic meals and menu options with limited food supplies; and
5. Easily-administered malnutrition screening assessments.
This toolkit is designed to be adaptable to a variety of emergency settings with or without an operational electronic medical record (EMR) system. That said, this toolkit is intended to expand over time to incorporate new protocol templates based on experiences faced by other nutrition personnel in emergency settings. As such, these tools should be considered templates that can be adapted for the nutrition personnel’s or clinician’s needs to best reconcile medical and nutrition records, harmonize patient information, and improve the continuity of care between medical and nutrition branches. We encourage those using this resource to collaborate with authors to expand this toolkit and help to improve this resource as preparedness planning tool for crisis nutrition personnel in future field hospital or humanitarian crisis settings.
Unless otherwise noted, the content in this toolkit is licensed under a CC BY-NC-SA 4.0.
1. Overview
During the novel coronavirus disease 19 (COVID-19) pandemic, countries worldwide have developed temporary medical facilities to provide sufficient testing and care to infected persons [1–5]. An extension of combat support hospitals and field hospitals, these facilities commonly provide emergency medical services during military deployment [6,7]. However, in recent years many countries have begun deploying these temporary hospitals to provide emergency services and supplies during natural disasters and humanitarian emergencies [8,9].
Throughout the COVID-19 pandemic, these facilities have faced growing volumes of infected persons and have lacked sufficient personnel, medical supplies, medical equipment, and bed capacity to effectively house and treat patients. Safety concerns for medical personnel have also inhibited the delivery of care by reducing patient interaction, wearing personal protective equipment, and performing medical assessments while practicing social distancing [10]. These challenges especially inhibit medical staff providing nutrition services where patient interaction is consistently needed to monitor nutrition status and deliver therapeutic meals multiple times per day during a patient’s hospital stay [10]. Furthermore, these nutrition operations require careful coordination and management of food contracts and supplies, which must be consistently monitored to ensure accessibility of patient meals and continuity of food safety, respectively.
In review of the Accreditation Council for Education in Nutrition and Dietetics’ Accreditation Standards for Nutrition and Dietetics Internship Programs, under ‘Domain 4. Practice Management and Use of Resources: Strategic application of principles of management and systems in the provision of services to individuals and organizations,’ training competencies lack mention of food contracts or the development of skills necessary to implement and sustain food contracts, which are becoming vital skills in response to COVID-19 [11]. Furthermore, these resources fail to provide sufficient training on managing food contracts, staffing nutrition personnel, recording patient nutrition status, or administering nutrition assessments in emergency or disaster relief efforts. Without these resources, nutrition personnel cannot sufficiently prepare for field hospital deployments and must modify existing nutrition assessments that are not designed for resource sparse settings. These challenges necessitate a central technical report created to inform nutrition protocols and assessments in emergency response settings for clinical nutritionists, dietitians, and personnel.
To promote preparedness plans for nutrition response in future humanitarian crises, we develop this Nutrition Response Toolkit for Humanitarian Crises to provide a standardize nutrition-focused protocols for implementation in future field hospital deployments or humanitarian emergency facilities. For each proposed tool, we explain that tool’s purpose and utilization, provide an example of how to implement this tool in the field, and provide a fillable form for use in crisis settings.
References
- Sisak, M. Many Field Hospitals Went Largely Unused, Will Be Shut Down. Military Times 2020.
- Mash, R.; Presence-Vollenhoven, M.; Adeniji, A.; Christoffels, R.; Doubell, K.; Eksteen, L.; Henrikse, A.; Hutton, L.; Jenkins, L.; Kapp, P.; et al. Evaluation of Patient Characteristics, Management and Outcomes for COVID-19 at District Hospitals in the Western Cape, South Africa: Descriptive Observational Study. BMJ Open 2021, 11, e047016–e047016, doi:10.1136/bmjopen-2020-047016.
- Francke, R.-L. Covid-19 Field Hospital Opens in Mitchells Plain. IOL News 2021.
- Canadian Press Ontario Says a COVID-19 Field Hospital Is Expected to Take Patients This Month. CTV News 2021.
- BBC Wales Covid-19: Are Field Hospitals Operating in Wales? BBC News 2020.
- Lewis, M.M.; Bower, A.; Cuyler, M.T.; Eden, R.; Harper, R.E.; Gonzalez Morganti, K.; Resnick, A.C.; Steiner, E.D.; Valdez, R.S. New Equipping Strategies for Combat Support Hospitals. RAND Health Quarterly 2012, 2, 2.
- LaBrecque, M.F.; Honsberger, M.A. Army Field Hospitals and Expeditionary Hospitalization; Army Sustainment Professional Bulletin; United States Army, 2018.
- Davis, L.E.; Rough, J.; Cecchine, G.; Schaefer, A.G.; Rohn, L.L. Hurricane Katrina: Lessons for Army Planning and Operations; RAND Corporation, 2007; p. 106.
- Larson, E.V.; Boling, B.; Eaton, D.; Genc, S.; Kravitz, D.; Leuschner, K.J.; Lewis, A.; Liggett, J.; Polley, L. U.S. Army North in the Hurricane Maria Response; RAND Corporation, 2020; p. 236.
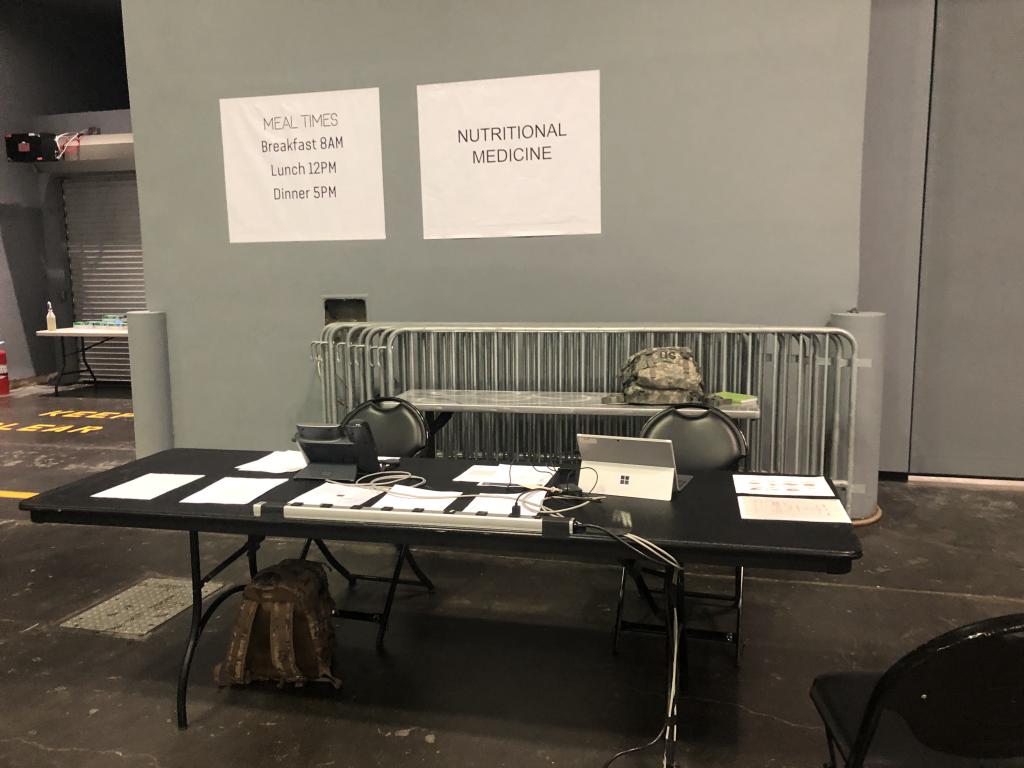
- Sanchez, E.; Gelfand, A.R.; Perkins, M.D.; Tarnas, M.C.; Simpson, R.B.; McGee, J.A.; Naumova, E.N. Providing Food and Nutrition Services during the COVID-19 Surge at the Javits New York Medical Station. In Review 2021.
- Accreditation Council for Education in Nutrition and Dietetics ACEND Accreditation Standards for Nutrition and Dietetics Internship Programs (DI); Academy of Nutrition and Dietetics, 2018.
This toolkit includes guidance for every step of staffing a field hospital, establishing nutrition-focused medical records, and monitoring patient nutrition status. Using this order of operations, we have designed the toolkit to have the following structure:
- Establishing a Field Hospital Nutrition Operations Team
- Staffing model for emergency settings
- Two-day staffer training program
- Monitoring Inpatient Nutrition Status
- Screener for inpatient nutrition status
- Modified ADIME note
- Tracker for patient census and diet orders
- Diet roster
- Receiving Nutrition Concerns from Field Hospital Staff
- Nutrition consultation form
- Diet order change and supplement request form
- Food temperature log
- Calculating Patient Nutrition Support Needs
- Guide for enteral formulary
- Enteral nutrition recommendation calculator
As the COVID-19 pandemic continues, we call upon the broader research and practice community, including the Academy of Nutrition and Dietetics, to develop guidelines for nutrition services in medical facilities. These guidelines must target training competencies for RDs, NDTRs, and other nutrition-related personnel providing medical care in field hospitals or emergency facilities during humanitarian crises. While the Nutrition Response Toolkit for Humanitarian Crises provides a foundation for such services, this toolkit must be expanded to enhance the scalability and generalizability of these tools for future emergency response efforts. This can only be done by collaborating with other medical and nutrition service professionals, who together can document shared and new experiences that warrant new tools for field response-related challenges. We welcome this future collaboration, and hope that these low-cost, easily-adaptable nutrition services and assessments tools can be aid nutrition personnel in future field hospital deployments and humanitarian emergencies.
The first draft of this toolkit was prepared by Emily Sanchez, MS, RD, CNSC of the Tufts University Friedman School of Nutrition Science and Policy and Army Medical Department Student Detachment, U.S. Army Medical Center of Excellence, Amy R. Gelfand, MS, RD, CNSC of the Bureau of Supplemental Food Programs, New York State Department of Health, Michael D. Perkins, MS, RDN of the Bureau of Supplemental Food Programs, New York State Department of Health, Maia C. Tarnas of the Community Research Initiative of New England, Ryan B. Simpson, MS of the Tufts University Friedman School of Nutrition Science and Policy, Jarrod A. McGee, FACHE, MHA, MBA of Army-Baylor University and the United States Army 1st Medical Brigade, William Beaumont Army Medical Center, and Dr. Elena N. Naumova of the Tufts University Friedman School of Nutrition Science and Policy.
The authors thank the Nutrition Operations Team and multi-agency collaborators at the Javits New York Medical Station, to include the New York State Department of Health, for their commitment to data collection in support of improving disaster response efforts for nutrition personnel.
Sanchez, E.; Gelfand, A.R.; Perkins, M.D.; Tarnas, M.C.; Simpson, R.B.; McGee, J.A.; Naumova, E.N. Nutrition Response Toolkit for Humanitarian Crises; Tufts Initiative for the Forecasting and Modeling of Infectious Diseases: Gerald J. and Dorothy R. Friedman School of Nutrition Science and Policy, Tufts University, 2021; https://sites.tufts.edu/naumovalabs/crisisnutritiontoolkit/.
2. Establishing a Field Hospital Nutrition Operations Team
When planning for a potential use of a field hospital, one must remember that field hospitals are modular medical treatment facilities generally designed to provide medical capabilities in a deployed setting [1]. Within the field hospital, it is the responsibility of nutrition care operations, which primarily consists of Registered Dietitians (RDs) and Nutrition Dietetics Technicians, Registered (NDTR), to provide services that include meal preparation and service to patients, medial nutrition therapy, dietetic planning and patient education [2]. Hospital food service and clinical nutrition operations are essential to ensure patients receive sufficient nutrition to prevent complications associated with malnutrition, while complying with the appropriate diet orders given their medical diagnosis [2]. Yet in the wake of a humanitarian crisis, no single staffing model exits for nutrition response in field hospitals [3]. With that in mind, we provide examples of a staffing model and personnel training program that can assist in establishing nutrition services within an emergency field hospital or medical facility.
References
- LaBrecque, M.F.; Honsberger, M.A. Army Field Hospitals and Expeditionary Hospitalization; Army Sustainment Professional Bulletin; United States Army, 2018
- United States Army Theater Hospitalization; Department of the Army: Headquarters, 2020.
- Joint Commission Surge Hospitals: Providing Safe Care in Emergencies; Joint Commission on Accreditation of Healthcare Organizations, 2006.
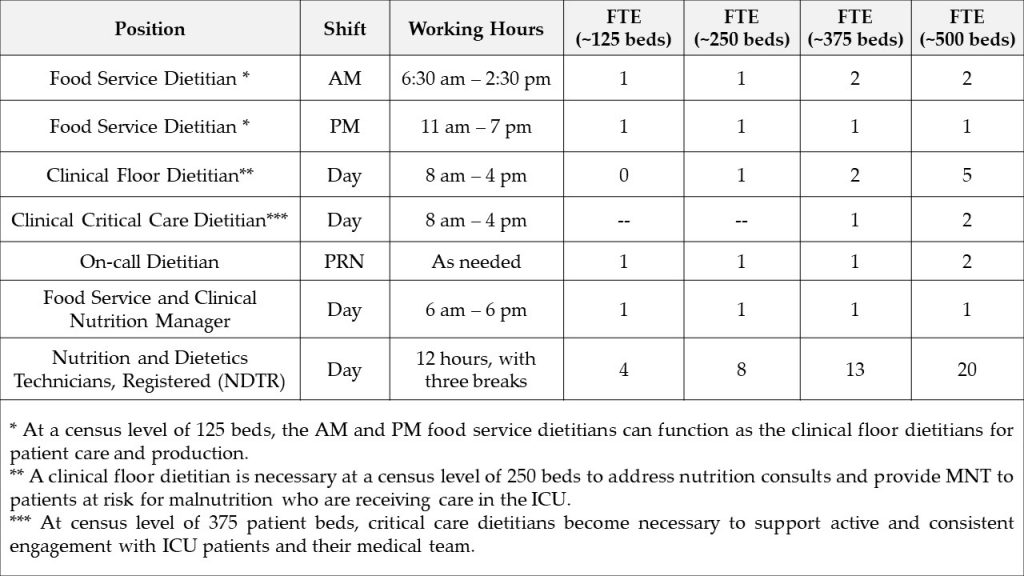
Purpose: The Field Hospital Staffing Model is designed to identify staffing needs for nutrition services in a field hospital or emergency facility setting with 125-500 patient beds. This model accommodates for extended time needed to complete patient assessments due to the absence of an EMR, donning and doffing full PPE, locating patients amid transfers, coordinating care with medical and nutritional personnel, documenting MNT recommendations, and balancing the completion of clinical and food service roles.
Utilization: This tool should be referenced during the planning phase of a field hospital mobilization. This model assumes that: i) nutrition operations are functional during a 12-hour period, e.g., 6:30 am – 6:30 pm, seven days per week; ii) the field hospital serves a patient census ranging from 125-500 patients per day; and iii) RDs have limited capacity (3-4 patients daily) to provide clinical care.
Example of a Field Hospital Staffing Model used at the Javits New York Medical Station from 28 April through 01 May of 2020:
Food Service Dietitians provide nutrition care to patients to prevent malnutrition and optimize recovery. Primary responsibilities include:
- AM Food Service Dietitian:
- Assessing menus and diet orders to ensure food items are appropriate
- Delivering meals safely at breakfast and lunch
- Confirming patient census, diet orders and creating diet production sheets
- Administering production sheets to NDTRs
- Supervising NDTRs preparing meal delivery carts
- Overseeing diet order and food allergy questions/concerns
- Answering questions regarding diet orders and assisting with appropriate food substitutions
- Implementing and maintaining adherence to food safety and equipment sanitation protocols
- Ensuring food waste is properly discarded after meal delivery service
- Checking floor nourishment par levels and confirming delivery of more stock items
- At census levels of <125 patients: assessing patients identified at risk for malnutrition high risk patients and providing nutrition consultations
- At census levels of <250 patients: assisting clinical floor dietitians as needed
- PM Food Service Dietitian:
- Assessing menus and diet orders to ensure food items are appropriate
- Delivering meals safely at dinner
- Confirming patient census, diet orders and updating diet production sheets for dinner
- Administering production sheets to NDTRs
- Supervising NDTRs preparing meal delivery carts
- Overseeing diet order and food allergy questions/concerns
- Answering questions regarding diet orders and assisting with appropriate food substitutions
- Implementing and maintaining adherence to food safety and equipment sanitation protocols
- Ensuring food waste is properly discarded after meal delivery service
- At census levels of <125 patients: assessing patients identified at risk for malnutrition high risk patients and providing nutrition consultations
- At census levels of <250 patients: assisting clinical floor dietitians as needed
Clinical Dietitians provide nutrition care to patients to prevent malnutrition and optimize recovery. Primary responsibilities include:
- Clinical Floor Dietitian:
- Providing nutrition care and management of patients in a general medicine setting
- Interpreting physician diet orders and modifying diet according to diet patterns and patient preferences
- Conducting clinical nutrition assessments on patients identified at risk for malnutrition via the Nutrition Screening Form (see Section 3. Monitoring Inpatient Nutrition Status) or the Nutrition Consult Form (see Section 4. Receiving Nutrition Concerns from Field Hospital Staff)
- Providing MNT recommendations (i.e., chronic disease management and strategies to improve food intake during hospital admission)
- Making appropriate recommendations for nutrition care including but not limited to:
- Oral supplements
- Nutrition supplements
- Food-drug interactions
- Communicating nutrition recommendations through appropriate medical documentation using the ADIME format
- Completing calorie counts
- Attending medical rounds and patient care plan meetings
- Coordinating care with patient’s primary care manager (PCM) and case management
- Communicating nutrition recommendations for assigned patients to food service staff
- Maintaining open communication between the hospital staff and Nutrition Operations
- Clinical Critical Care Dietitian:
- Conducting nutrition assessment on patients in the ICU
- Interpreting physician diet orders and modifying diet according to diet patterns and patient preferences
- Conducting clinical nutrition assessments on patients identified at risk for malnutrition via the Nutrition Screening Form (see Section 3. Monitoring Inpatient Nutrition Status) or the Nutrition Consult Form (see Section 4. Receiving Nutrition Concerns from Field Hospital Staff)
- Providing medical nutrition therapy recommendations including but not limited to:
- Enteral nutrition support
- Parenteral nutrition support
- Oral supplements
- Nutrition supplements
- Food-drug interactions
- Communicating nutrition recommendations through appropriate medical documentation using the ADIME format (see Section 3. Monitoring Inpatient Nutrition Status)
- Attending medical rounds and patient care plan meetings with ICU team
- Coordinating care with patient’s PCM and case management
- Performing patient handoff to floor dietitian if patient transferred out of the ICU
On-Call Dietitians serve as backup dietitians in the event of an illness or emergency. On-call dietitians share the responsibilities of food service and clinical dietitians.
Food Service and Clinical Nutrition Manager provides leadership, oversight and direction to both the food service and clinical staff. Primary responsibilities include:
-
- Attending field hospital leadership and operations meetings and monitoring staffing needs
- Assessing menus and diet orders to ensure food items are appropriate
- Leading the administration and coordination of the food service contract with the onsite vendor
- Working with vendor, clinical staff, and field hospital leadership to assess and coordinate procurement of patient meals
- Coordinating with vendors and production dietitians to assess appropriateness of food items for each diet order and obtaining allergen information for each food item
- Leading communications with the clinical dietitians and assessing ongoing staffing needs
- Ensuring adherence to food safety and clinical nutrition policies
Nutrition and Dietetics Technicians, Registered (NDTR) provide nutrition care to patients to prevent malnutrition and optimize recovery. Primary responsibilities include:
-
- Performing malnutrition screening using the Nutrition Screening Form and referring patient to a clinical dietitian as needed
- Collecting data on the patient’s dietary preferences, food allergies and/or intolerances
- Verifying diet ward rosters before each meal delivery
- Communicating roster updates to food service dietitians
- Preparing patient meal delivery carts
- Delivering patient meals
- Following food safety and equipment sanitation protocols
- Supporting maintenance of Patient Census and Diet Order Tracker (see Section 3. Monitoring Inpatient Nutrition Status)
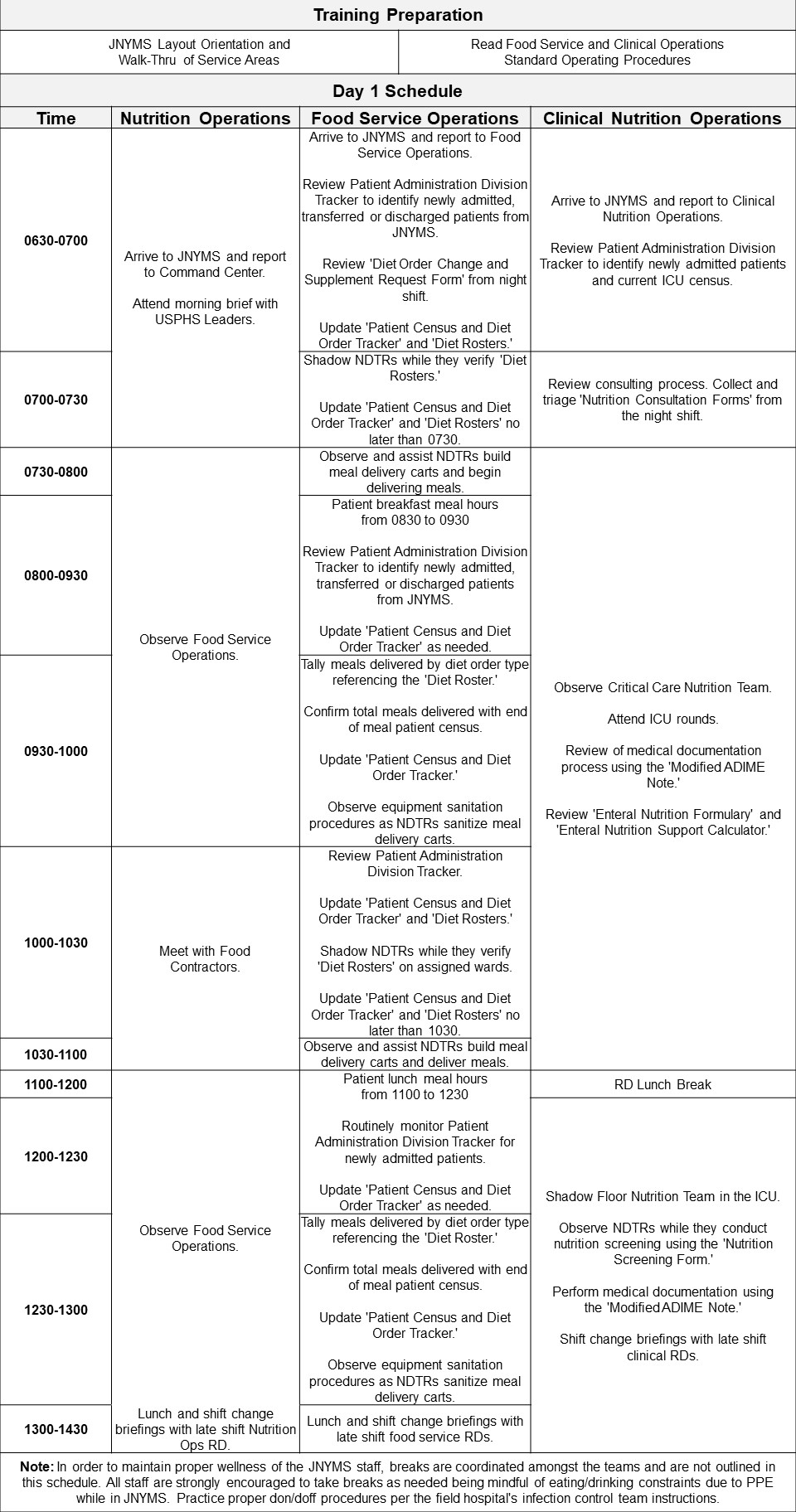
Purpose: The Training Program Syllabus is designed to orient new RDs and offer appropriate training on food service management, clinical nutrition, and nutrition support operations. These trainings should explain the organization of the field hospital, operational mandate for nutrition services, and coordinated protocol for simultaneously managing food services and performing clinical nutrition evaluations.
Utilization: This tool should be referenced during the planning phase of field hospital mobilizations and when onboarding new RDs. This comprehensive two-day training resource helps orient civilian RDs and offer appropriate training on food service management, clinical nutrition, and nutrition support operations for RDs who lack sufficient clinical experience.
Example of Training Program Syllabus used at the Javits New York Medical Station from 28 April through 01 May of 2020:
3. Monitoring Inpatient Nutrition Status
Designed to improve the consistency and quality of individualized care for patients, RDs follow the Nutrition Care Process (NCP), established by the Academy of Nutrition and Dietetics (AND) that includes a Nutrition Assessment, Nutrition Diagnosis, Nutrition Intervention, and Nutrition Monitoring and Evaluation steps [1,2]. Specifically, Nutrition Monitoring and Evaluation is used to determine and measure the amount of progress made for the nutrition intervention and whether the nutrition related goals and expected outcomes are being met [3]. In order to assess such progress, RDs will frequently reference the patient’s EMR; however, access to such systems is not always possible in humanitarian crises despite their importance in disaster-related medical responses [4–6]. We provide these tools to improve the resilience and continuity of care of health services using easily-adapted, ready-to-use patient nutrition status screeners, trackers, and nutrition status assessments.
References
- AND Nutrition Care Process Available online: https://www.andeal.org/ncp (accessed on 3 May 2021).
- The Academy Quality Management Committee Academy of Nutrition and Dietetics: Revised 2017 Scope of Practice for the Registered Dietitian Nutritionist. Journal of the Academy of Nutrition and Dietetics 2017, 118, 141–165, doi:10.1016/j.jand.2017.10.002.
- AND NCP Step 4: Nutrition Monitoring and Evaluation 2018.
- Horahan, K.; Morchel, H.; Raheem, M.; Stevens, L.; Pawlak, S. Electronic Health Records Access during a Disaster. 1 2014, 5, doi:10.5210/ojphi.v5i3.4826.
- Oza, S.; Jazayeri, D.; Teich, J.M.; Ball, E.; Nankubuge, P.A.; Rwebembera, J.; Wing, K.; Sesay, A.A.; Kanter, A.S.; Ramos, G.D.; et al. Development and Deployment of the OpenMRS-Ebola Electronic Health Record System for an Ebola Treatment Center in Sierra Leone. J Med Internet Res 2017, 19, e294, doi:10.2196/jmir.7881.
- deRiel, E.; Puttkammer, N.; Hyppolite, N.; Diallo, J.; Wagner, S.; Honoré, J.G.; Balan, J.G.; Celestin, N.; Vallès, J.S.; Duval, N.; et al. Success Factors for Implementing and Sustaining a Mature Electronic Medical Record in a Low-Resource Setting: A Case Study of ISanté in Haiti. Health Policy and Planning 2017, 33, 237–246, doi:10.1093/heapol/czx171.
Purpose: The Nutrition Screening Form is designed to collect nutrition-related information on all inpatients as efficiently as possible. This form was adapted from the Mini Nutritional Assessment and Subjective Global Assessment screening tools [1-3]. Questions specifically target the patients’ ability to chew and swallow, food preferences, and food allergies to inform the composition and texture of therapeutic meals that patient receives.
Utilization: Prior to use, update the following fields:
- ‘eFIND#’ to the field hospital’s/emergency facility’s medical record numbering system
- ‘Pod #’ to the field hospital’s/emergency facility’s ward or floor division structure
This form can be used for initial and reassessment interviews by NTDRs to identify individuals at risk for malnutrition. A patient is classified as at risk for malnutrition and referred to a clinical dietitian if they report a ‘fair’ or ‘poor appetite’ appetite history and a ‘recent’ and ‘unintentional’ weight loss history. Patient-reported chewing or swallowing difficulties, cultural/religious food preferences, and food allergies should be communicated to food service staff. This information should also be updated on the Patient Census and Diet Order Tracker (see Tracker for patient census and diet orders below).
Download: A PDF fillable version of the Nutrition Screening Form can be found here!
Example of Nutrition Screening Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
References
- MNA Mini Nutritional Assessment (MNA) 2009.
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment Short-Form (MNA-SF): A Practical Tool for Identification of Nutritional Status. J Nutr Health Aging 2009, 13, 782–788, doi:10.1007/s12603-009-0214-7.
- Detsky, A.S.; McLaughlin; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What Is Subjective Global Assessment of Nutritional Status? Journal of Parenteral and Enteral Nutrition 1987, 11, 8–13, doi:https://doi.org/10.1177/014860718701100108.
Purpose: The Modified ADIME Note was adapted from Standardized Form 600: Chronological Record of Medical Care and the Nutrition Care Process note writing style [1–3]. ADIME stands for Assessment, Diagnosis, Intervention, Monitoring, and Evaluation – a five step process for examining the nutrition status of a patient. In the absence of an EMR, this reporting format prioritizes the assessment, diagnosis, and intervention components of ADIME, and enhances medical documentation efficiency.
Utilization: Prior to use, update the ‘eFIND#’ to the field hospital’s medical record numbering system. After providing individual MNT, clinical RDs should document their nutrition assessment, diagnosis, and intervention plan and recommendations using the Modified ADIME Note. This document should be placed into the patient’s medical record and steps should be taken to communicate nutrition recommendations with the patient’s primary care manager to optimize continuity of care.
Download: A PDF fillable version of the Modified ADIME Note Form can be found here!
Example of Modified ADIME Note Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
References
- US General Services Administration Standard Form 600: Chronological Record of Medical Care.
- Lacey, K.; Pritchett, E. Nutrition Care Process and Model: ADA Adopts Road Map to Quality Care and Outcomes Management. J Am Diet Assoc 2003, 103, 1061–1072, doi:10.1016/s0002-8223(03)00971-4.
- Thompson, K.L.; Davidson, P.; Swan, W.I.; Hand, R.K.; Rising, C.; Dunn, A.V.; Lewis, N.; Murphy, W.J. Nutrition Care Process Chains: The “Missing Link” between Research and Evidence-Based Practice. J Acad Nutr Diet 2015, 115, 1491–1498, doi:10.1016/j.jand.2015.04.014.
Purpose: The Patient Census and Diet Order Tracker is designed to facilitate meal forecasting in a disaster response setting. This is done by recording the number of patients consuming different types of meals over pre-determined mealtimes in a field hospital. Daily and weekly tallies of delivered meals can be used to estimate the popularity of food supplies in the patient population. This tracker also serves as a quality control tool in which the total number of meals delivered per food service period (e.g., breakfast, lunch, and dinner) can be matched to the current patient census.
Utilization: This tool is available as a weekly hard-copy tracker or as a modifiable Excel file. Prior to use, update the following fields:
- ‘Diet Orders’ to reflect the diet order types available at the field hospital; and
- ‘Date’ to ensure that the start date of each week is the day that meal forecasts must be distributed to the food suppliers.
This tracker carefully integrates with diet order and food allergy information to serve as a monitoring tool for successful and accurate meal delivery. This is done by recording the number of persons served for breakfast, lunch, and dinner according to each diet order. After each week, total meals served provides an estimate of the number of meals needed for the next week. This inventory assessment helps maintain adequate forecasting of supplies with food contractors. Additionally, this tool helps maintain proper food safety assurance and meal delivery coverage in accordance with USPHS Food Safety regulations.
Download: An Excel fillable calculator of the Patient Census and Diet Order Tracker can be found here!
Example of Patient Census and Diet Order Tracker used at the Javits New York Medical Station from 28 April through 01 May of 2020:
To best use this tracker, we recommend the following:
- One hour prior to meal delivery, personnel charged with delivering meals to patients should update the ‘Total Census' with the total number of patients in the hospital (Example A).
- The tracker should then be distributed to food service personnel responsible for producing and supplying meals to inpatients.
- Food service personnel should calculate the correct quantity and type of meals by multiplying the total patient census and the percentage of orders per diet order type. Food service personnel will then package, store, and deliver meals in accordance with standard processes.
- Within 30 minutes of meal delivery to patients, meal delivery personnel should:
- Tally diet orders per hospital ward to provide a total number of meals served by diet order type.
- Update the tracker with the total number of meals distributed to all patients.
- Compare the alignment of total 'Meals Served' to the 'Total Census’ (Example A).
- In the Excel version, ‘Meals Served’ auto calculates the sum of all meals delivered by diet order type to an aggregate total.
- Discrepancies between meals served and patient census totals should be addressed by food service personnel in the following ways:
- If fewer meals than the total census were served:
- Verify the current hospital census at the end of the meal period and identify if patients were discharged from the hospital during meal delivery.
- Verify diet ward rosters to ensure that all patients identified at the beginning of the meal period received a meal.
After delivering all meals, nutrition operations personnel should identify new hospital admissions during meal delivery and provide appropriate meal options in accordance with medical and nutritional prognoses.
- If more meals than the total census were served:
- Identify if and how many double-portion diet orders were placed by medical or nutritional staff.
- Provide a note indicating which patient(s) received double portions to properly adjust diet order tallies.
- Once all daily values are verified, report the sum of all ‘Meals Served’ and ‘Diet Orders’ in the ‘Weekly Totals’ column (Example B).
- In the Excel version, 'Weekly Totals' for 'Meals Served' and ‘Diet Orders’ will auto-populate.
- Distribute the completed tracker to food suppliers once data have been finalized on the seventh day of the weekly cycle.
- Calculate the ‘% of Meals Served’ per diet order by dividing the ‘Weekly Totals for Diet Order 1’ by the ‘Weekly Total of Meals Served’ and multiplying the output by 100.
- The sum of all the ‘% of Meals Served’ should total 100%
- Use the product of the '% of Meals Served’ and weekly total of each diet order to facilitate meal forecasting for the following weekly cycle.
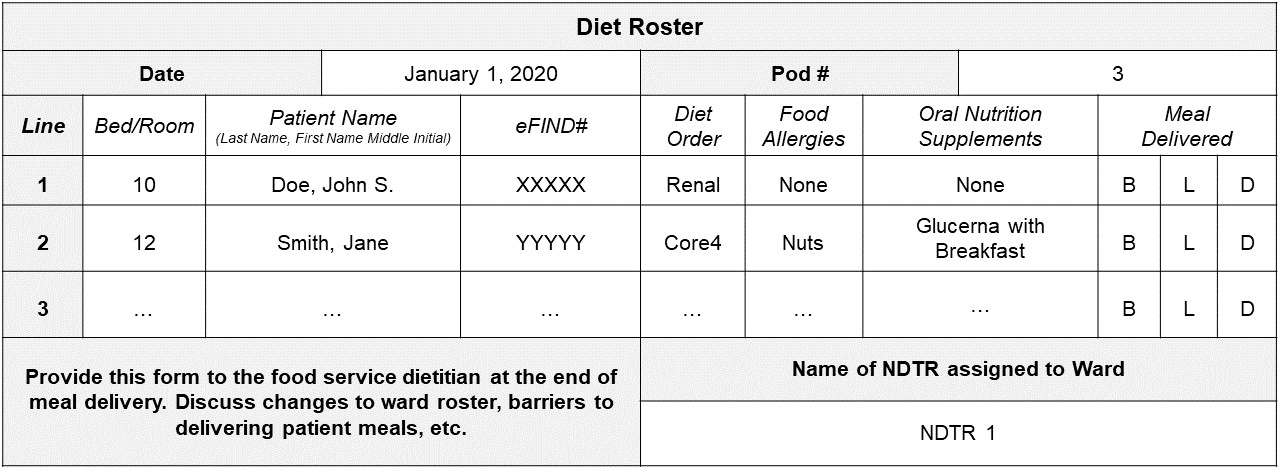
Purpose: The Diet Roster is designed to quickly identify patients’ diet orders, food allergies, and oral nutrition supplement requirements during meal delivery. The roster should be completed for every patient ward or floor by the assigned NDTR. This form should be reviewed and updated regularly as patients are admitted and discharged.
Utilization: First, update the ‘eFIND#’ to the field hospital’s medical record numbering system. Prior to meal delivery, NDTRs should review the patient’s medical record to verify their diet order, food allergy information, and oral nutrition supplement requirements. This information should be transcribed onto the diet roster. This form is then referenced when building patient meal delivery carts. After the patient meal is delivered, NDTRs cross off the appropriate ‘Meal Delivered’ column (‘B’ for breakfast, ‘L’ for lunch, and ‘D’ for dinner). After all patients on the assigned ward or floor have received a meal, the NDTR submits the roster to the food service dietitian. The food service dietitian then uses the roster to:
- Determine the number of meals delivered per meal period (to be used in the Patient Census and Diet Order Tracker shown above)
- Update the Patient Census and Diet Order Tracker with changes to diet orders or oral nutrition supplement requirements and food allergy information
Download: A PDF fillable version of the Diet Roster Form can be found here!
Example of Modified ADIME Note Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
4. Receiving Nutrition Concerns from Field Hospital Staff
Registered Dietitians frequently work hand-in-hand with primary care providers as part of a multidisciplinary healthcare team to deliver coordinated care. RDs are an integral part of a patient’s health care, as they are trained to assess the nutrition-related health needs of patients, considering other factors affecting nutrition and health status (e.g., culture, ethnicity, and social determinants of health), provide nutrition counseling and nutrition education to optimize nutritional status, prevent disease, or maintain and/or improve health and well-being [1]. Research has shown consulting a RD in primary care settings appear effective for improving diet quality, diabetes outcomes, and weight loss outcomes [2]. However, additional studies have found low referral rates from primary care clinicians to a RD amongst the most vulnerable patients such as those at risk of malnutrition [3].
References
- The Academy Quality Management Committee Academy of Nutrition and Dietetics: Revised 2017 Scope of Practice for the Registered Dietitian Nutritionist. Journal of the Academy of Nutrition and Dietetics 2017, 118, 141–165, doi:10.1016/j.jand.2017.10.002.
- Mitchell, L.J.; Ball, L.E.; Ross, L.J.; Barnes, K.A.; Williams, L.T. Effectiveness of Dietetic Consultations in Primary Health Care: A Systematic Review of Randomized Controlled Trials. J Acad Nutr Diet 2017, 117, 1941–1962, doi:10.1016/j.jand.2017.06.364.
- Eglseer, D.; Bauer, S. Predictors of Dietitian Referrals in Hospitals. Nutrients 2020, 12, doi:10.3390/nu12092863.
Purpose: The Nutrition Consultation Form is designed to streamline requests from the patient’s primary care manager or nursing team for nutrition consultation by a clinical RD. This consultation is designed to be conducted with limited contact time (<5 minutes), performed at a distance (to accommodate medical personnel safety), and integrate assessments, recommendations, and educational needs within the same form.
Utilization: Prior to use, update the ‘eFIND#’ to the field hospital’s medical record numbering system. The patient’s primary care manager or nursing team should complete the Nutrition Consultation Form when requesting nutrition assessment or education from a clinical RD.
Download: A PDF fillable version of the Nutrition Consultation Form can be found here!
Example of Nutrition Consultation Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
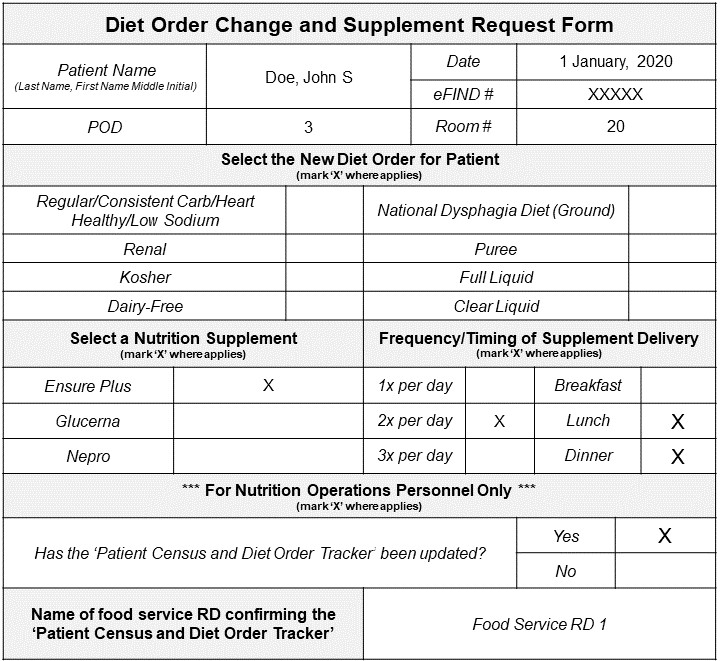
Purpose: The Diet Order Change and Supplement Request Form is designed to streamline changes in diet orders and/or oral nutrition supplements requested by the patient’s primary care manager. This is of particular importance if a field hospital lacks an EMR for recording patient nutrition and medical status. Furthermore, such a form can ensure that therapeutic meals reconcile with medical prognoses and treatments.
Utilization: Prior to use, update the ‘eFIND#’ to the field hospital’s medical record numbering system. The patient’s primary care manager should complete the Diet Order Change and Supplement Request Form following a new diet order and/or prescription for an oral nutrition supplement. If an oral nutrition supplement is selected, the frequency and timing of supplement delivery must also be selected. This form is then submitted to Nutrition Operations personnel or the designated personnel’s mailbox. Food service dietitians then update the Patient Census and Diet Order Tracker with the changes.
Download: A PDF fillable version of the Diet Order Change and Supplement Request Form can be found here!
Example of Diet Order Change and Supplement Request Form used at the Javits New York Medical Station from 28 April through 01 May of 2020:
Purpose: The Food Temperature Log is designed to monitor and record food temperatures to ensure food is safe when stored, prepared, and served. This is of particular importance when meal preparation occurs at an off-site facility and must be transported to the field hospital for before each meal delivery.
Utilization: One log is needed per day of patient meal delivery. Nutrition staff and personnel should perform temperature checks on a predetermined sample proportion of meals and/or food items per meal period. If there is a discrepancy between the temperature taken and the appropriate temperature to maintain food safety, the food service dietitian is alerted and implements a corrective action.
- Appropriate cold chain management: ≤41°F (5°C)
- Appropriate hot chain management: >135°F (57°C)
Download: A PDF fillable version of the Food Temperature Log Form can be found here!
Example of Food Temperature Log used at the Javits New York Medical Station from 28 April through 01 May of 2020:
5. Calculating Patient Nutrition Support Needs
The scope of practice for RDs also includes the ordering and monitoring of nutrition interventions to meet estimated nutrient and energy needs, including but not limited to prescribed diets, medical foods, dietary supplements, and nutrition support therapies (i.e., enteral nutrition support) [1]. The Academy of Nutrition and Dietetics offers few calculators, via the ‘Nutrition Care Manual,’ to estimate a body mass index and energy requirements or perform metric conversions, which are essential to the NCP [2]. However, a gap exists for similar tools when calculating a patient’s nutrition support needs. The American Society of Parenteral and Enteral Nutrition does offer an algorithmic practice tools to aid decisions surrounding the appropriateness of nutrition support therapies, but, yet again, a practice tool or calculator for the everyday clinician is missing [3].
References
- The Academy Quality Management Committee Academy of Nutrition and Dietetics: Revised 2017 Scope of Practice for the Registered Dietitian Nutritionist. Journal of the Academy of Nutrition and Dietetics 2017, 118, 141–165, doi:10.1016/j.jand.2017.10.002.
- AND Nutrition Care Manual 2020.
- ASPEN Nutrition Care Algorithm Available online: https://www.nutritioncare.org/Guidelines_and_Clinical_Resources/Toolkits/Malnutrition_Toolkit/Nutrition_Care_Algorithm/.
Purpose: The Enteral Nutrition Formulary Guide is designed to provide a comprehensive overview of nutrition information provided by oral nutrition supplements, enteral nutrition formulas, and modulars. This tool is provided to help identify key macronutrient and micronutrient levels in each supplement, formula, or modular for calculating recommended doses.
Utilization: This tool is available as a modifiable Excel file. Prior to use, update this formulary based on available oral nutrition supplements, enteral nutrition formulas, and modulars. This information can often be found on the product’s nutrition facts label or from the supplier’s website. Once updated, this tool should be referenced when calculating a patient’s estimated nutrient requirements and when discussing available oral nutrition supplements, enteral nutrition formulas and modulars with other healthcare professionals.
Download: An Excel fillable calculator of the Enteral Nutrition Formulary Guide can be found here!
Example of Enteral Nutrition Formulary Guide used at the Javits New York Medical Station from 28 April through 01 May of 2020:
Purpose: The Enteral Nutrition Support Calculator is designed to support RDs when calculating the provision of calories, protein, and fluid for various enteral nutrition formulas. This calculator is meant to provide a quick reference for field hospital clinical nutrition staff and aims to improve efficiency and reduce errors when estimating patients’ nutrition support requirements. Details on nutrient provision should be ascertained from the enteral nutrition formula’s manufacturer’s website.
Utilization: This tool is available as a modifiable Excel file. Prior to use, update the Enteral Nutrition Formulary Guide from above for a quick reference when completing ‘Part B: Select enteral nutrition formula’.
Download: An Excel fillable calculator of the Enteral Nutrition Support Calculator can be found here!
Example of Enteral Nutrition Formulary Guide used at the Javits New York Medical Station from 28 April through 01 May of 2020:
To best use this calculator, we recommend the following:
- Convert the patient's weight from pounds to kilograms in ‘Part A: Re-calculate patient weight.’ This step must be completed to calculate the calories and protein provided by formulary per kilogram patient weight in ‘Part D: Calculate enteral nutrition support recommendations.’
- Enter the patient's weight in pounds in the yellow cell to convert the weight from pounds to kilograms (calculated in adjacent white cell).
- Update ‘Part B: Select enteral nutrition formula’ with information from the Enteral Nutrition Formulary Guide from above. The information entered in the yellow cells includes:
- Calories provided per milliliter of selected formula;
- Protein provided per liter of the selected formula;
- Water provided per lit of the selected formula; and
- Milliliters of formula per container of the selected formula.
- Update ‘Part C: Recommend hourly rate and length of admission’ with your recommended hourly rate and total hours of administration per day to auto calculate the 'Total Volume (mL)' of enteral nutrition provided per day. The information entered in the yellow cells includes:
- The recommended hourly rate of enteral nutrition administration; and
- The recommended total hours of enteral nutrition formula administration per day.
- Review the auto calculations performed in 'Part D: Calculate enteral nutrition support recommendations', which include:
- 'Calories per Day (kcal/d)’ calculated as the product of the total volume of formula delivered from ‘Part C: Recommend hourly rate and length of admission’ and the calories per milliliter of enteral nutrition formula from ‘Part B: Select enteral nutrition formula;’
- 'Calories per Patient Weight (kcal/kg patient)’ calculated as the quotient of the ‘Calories Per Day (kcal/d)’ calculated above and the patient weight in kilograms from ‘Part A: Re-calculate patient weight;’
- 'Protein per Day (g protein/d)’ calculated as the product of the protein per one liter (or one thousand milliliters) formula from ‘Part B: Select enteral nutrition formula’ and the total volume of formula delivered from ‘Part C: Recommend hourly rate and length of admission;’
- 'Protein per Patient Weight (g protein/kg patient)’ calculated as the quotient of the ‘Protein Per Day (g protein/d)’ calculated above and the patient weight in kilograms from ‘Part A: Re-calculate patient weight;’
- 'Water per Day (mL water/d)’ calculated as the product of the water per one liter formula (or one thousand milliliters) from ‘Part B: Select enteral nutrition formula’ and the total volume of formula delivered from ‘Part C: Recommend hourly rate and length of admission;’ and
- 'Containers Formula per Day (containers/d)’ calculated as the quotient of the total volume of formula delivered from ‘Part C: Recommend hourly rate and length of admission’ and the total volume of the formula per container from ‘Part B: Select enteral nutrition formula.’
- Communicate nutrition support recommendations, specifically the number of cartons or liters recommended for your patient, to food service personnel tasked with delivering meals. Limit enteral nutrition support recommendations to only the calculations appropriate for your available enteral nutrition formulary.