Breast cancer is the most frequently diagnosed type of cancer and the leading cause of cancer-related deaths among women. (Waks & Winer, 2019). About 20% of breast cancers are classified as triple negative, meaning they test negative for the expression of estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2). (Hudis et al. 2011). The lack of molecular markers in TNBC makes it particularly difficult to treat, as these typically serve as therapeutic targets. The disease has a poor prognosis, and those with TNBC have a shorter median life expectancy than patients with other forms of breast cancer (Waks & Winer, 2019). The disease has a 5 year survival rate of 40%. (Yavuz et al. 2022).
Metastasis is the process by which cancer cells leave the original tumor site, disseminate to a foreign tissue, and colonize in a new site to form a new tumor. Metastasis drastically decreases the overall survival rate and results in greater systemic effects of the disease. (Yao et al. 2019). One way to reduce metastasis is through the use of targeted therapies. These were first introduced with the approval of the breast cancer drug tamoxifen in 1998. (Lippman & Brown, 1999). Targeted therapies work by silencing or inhibiting malignant signaling pathways that are associated with the expression of the cancer phenotype. The uncovering of more and more targeted therapies allow for a wider range of cancer mutations to be mitigated. This provides incremental progress towards a definitive cure for the disease. However, this progress is inherently reliant on the detailed understanding of the effects of gene expression on cell behavior. These systems must be investigated thoroughly in order to elucidate an avenue for effective therapeutic intervention.
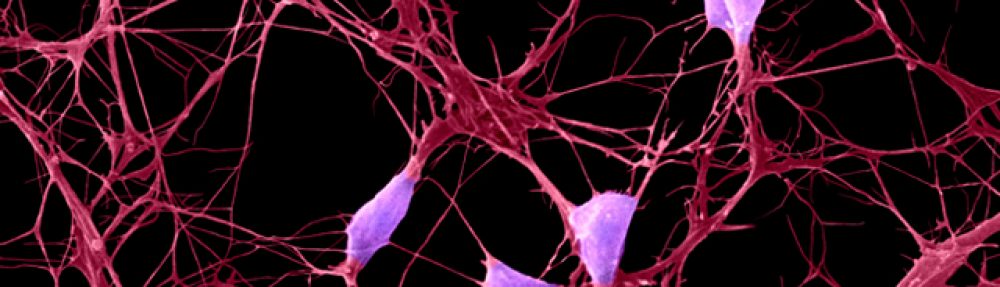
Our project is specifically investigating the role of neuronal gene expression in TNBC cells. Preliminary data has shown that the genes β3-tubulin (TUBB3) and microtubule-associated protein Tau (MAPT) are associated with increased metastatic potential of TNBC. This correlation suggests that these genes play a significant role in the progression of TNBC. Likewise, they could serve as therapeutic targets. To investigate these genes, we plan to first create a knockdown protocol. CRISPR and siRNA are the two most common ways to silence a gene in-vitro. Each of these requires its own set of optimization and quality assurance procedures. Additionally, they are better suited for different scenarios, which is best determined experimentally. The knockdown method will allow us to genetically engineer a platform that will allow us to study the gene’s effect on the malignancy of breast cancer. We plan to investigate how the genes affect cancer cells’ ability to metastasize by looking at differences in proliferation rate, migratory behavior, and cell morphology. We also plan to look at how chemotherapy affects the viability and morphology of cancer cells after knockdown of these genes. Lastly, we plan to validate and generalize these findings by repeating the experiments in multiple cell lines.