Reduced γ-Aminobutyric Acid in Occipital and Anterior Cingulate Cortices in Primary Insomnia: a Link to Major Depressive Disorder? (30)
Introduction: The paper analyzes the suggestion that the reduction of γ-aminobutric acid (GABA) plays a primary role both in major depressive disorder (MDD) and primary insomnia (PI). The paper uncovered that PI subjects were found to have significantly lower GABA/Cr in the occipital cortex (OC) when compared to healthy sleeper comparison subjects
Background: Insomnia has been noted as the most common sleep complaint within industrialized countries, causing significant daytime consequences within the adult population. Insomnia is thought to be linked to major depressive disorder (MDD), as those suffering PI have an increased risk of developing MDD. Gamma-aminobutyric acid (GABA) is the primary neurotransmitter in the central nervous system (CNS) and has been noted to have a role in the maintenance of insomnia. Furthermore, PI patients are found to have elevated levels of arousal, indicating a decrease in inhibitory GABAergic neurotransmission. In association with previous treatment of receptor agonists (BRZAs), which promote sleep by increasing receptor affinity for GABA, it can be hypothesized that GABA plays an integral role in the etiology of PI
Methods: The researchers implemented proton magnetic resonance spectroscopy (1H-MRS) in order to identify if there was a decrease in global brain GABA in PI (Fig. 1). The primary aim of the study was to examine brain GABA using single-voxel 1H-MRS at high field (4 Tesla) within the thalamus, occipital cortex (OC), and anterior cingulate cortex (ACC), relative to healthy controls
- PI subjects met the criteria of PI enlisted within the DSM-IV
- Age and sex-matched control subjects
Sleep Diaries: Subjects completed sleep-wake diaries for 2 weeks (including sleep-wake parameters, substance use, and sleep quality)
MR imaging: Imaging and spectroscopy was performed on a whole-body 4-Tesla MR scanner
Proton MRS: Proton spectroscopy implemented a GABA-optimized MEGAPRESS sequence (derived from Mescher et al, 1998).
Beck’s Depressive Inventory: A 21-question multiple-choice self-report survey that measures the severity of depression
Fig 1: Point Resolved Spectroscopy with MEGAPRESS with GABA difference-edited spectrum from the OC of a study subject. Metabolites also included within the analysis include creatine (Cr), myo-inositol (ml), total choline (Cho), N-acetyl aspartate (NAA), glutamate (Glu), glutamine plus glutamate (Glx) and GABA (30)
Results of Demographics and Sleep-wake Measures for PI and Controls: Beck Depression Inventory (BDI) was found to be significantly higher in PI than in the control, however below the threshold for clinical mood disorder classification.
Results of GABA/Cr concentration in PI and Control: PI subjects had significantly reduced GABA/Cr levels compared to controls in the OC (p=0.0005) and ACC (p=0.03) (Fig.2). Those who reported taking sedative-hypnotics did not alter the findings in either OC or ACC. Two-way ANOVA was used to determine if a sex difference was noted within the PI group, yielding no significant effect of sex (Table 1).
Figure 2. GABA/Cr concentration of control and PI group within OC, ACC, and Thal. Solid lines indicate group means (30)
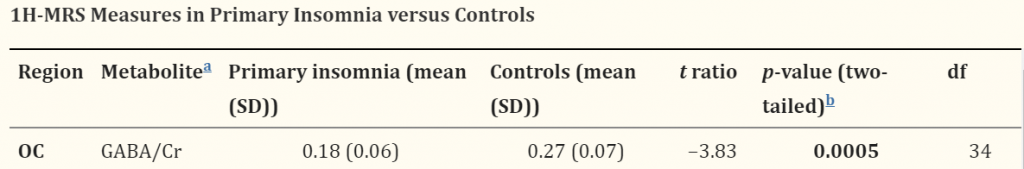
Table 1. GABA/Cr concentration in OC region analyzed through 1H-MRS in PI versus Control (30)

Conclusion: Findings illustrate that there is reduced brain GABA in PI participants within the OC and ACC brain regions (Table 1, 2). GABA/Cr levels in Thal were found to be not significant between PI and control. Findings aid in the identification of the neurobiology of insomnia, and potential areas that are more susceptible to GABA reduction within the PI population. The study also concludes that PI is not necessarily associated with MDD, however, there seems to be a positive correlation between the two disorders (in vivo studies have identified MDD participants have decreased GABA in prefrontal regions and OC). Reduction of GABA in shared brain regions within PI and MDD populations suggests that there may be a common neurochemical alteration within these disorders. An interesting prospective study that could be derived from the paper’s results is the potential to treat insomnia patients with SSRIs such as Fluoxetine or Citalopram, which are currently used to help those with MDD.
Very well summarized and report of the paper! It is very easy for me to follow every single detail of the paper and I fully understood what the paper is about. One minor suggestion that I would give is elaborate on what Beck Depression Inventory is. I do not know what Beck Depression Inventory is higher in patient with PI means. Well done.
Heard. Included
I like how this page is broken down into the different sections of the paper. These sections are nicely summarized, and the figures were helpful in supplementing the results/conclusions. One thing of note, figure 1 is a bit blurry because of how zoomed-in it is. It would be nicer as a higher resolution picture if possible, even if it’s a bit smaller. Good job!
You do a nice job discussing this paper but it would be great for you to talk about some questions you had after reading the data and where the research could lead next.
Heard! Included
I really like this page. The bolded subsections are great, and really help the reader follow along with your analysis of the page. Honestly, I have no major suggestions.
Nice work here! I think you did a great job writing the conclusion and putting together a good summary of the main themes of the paper. I also think the selection of this paper was great as it closely relates to the topics covered in the other webpages. You could do a bit more discussion on the actual data itself, summarizing what the obtained values were and exactly what those values mean in relation to the conclusions made.