No Treatment for Negative Symptoms?
“You really have to look for sad mood to identify depression,” says Douglas Noorsdy, Associate Professor of Psychiatry at Dartmouth University. “Patients with schizophrenia will usually describe a lack of emotional expression and a blah feeling, whereas in depression they’ll have an actively depressed mood.”

Negative symptoms: A decrease or loss of normal functions, such as a loss of energy, motivation, and emotional display of affect
This lack of emotional expression and “blah feeling” that Dr. Noorsdy is describing is an example of the problematic domain of signs and symptoms of schizophrenia called negative symptoms. As I have explained in my first blog post, the “negative symptom” terminology refers to a decrease or loss of normal functions, such as a loss of energy, motivation, and emotional display of affect. Here, it is important to distinguish between lack of expression and lack of feeling because when questioned, patients with schizophrenia often express a full range of feelings and desires (Kring et al., 1993). The difference between what they may feel and what they show has to be taken into account in deciding whether or not the patient is suffering from depression or from the negative symptoms of schizophrenia.
According to the Harvard Medical School’s Family Health Guide on Schizophrenia, “negative symptoms tend to be more stable than positive symptoms, and commonly begin to emerge very early in the course of schizophrenia, even before the development of positive symptoms.” In fact, negative symptoms often first appear during the prodromal phase of schizophrenia. During this phase, which can last weeks or months, people start to withdraw from friends and family members and begin to lose interest in their usual pursuits. Hence, emotion deficits characterize this period and tend to be misunderstood as signs of laziness rather than illness.
In this blog post, the question I will aim to answer is: How debilitating are these negative symptoms and how effective are currently prescribed antipsychotics in their treatment?
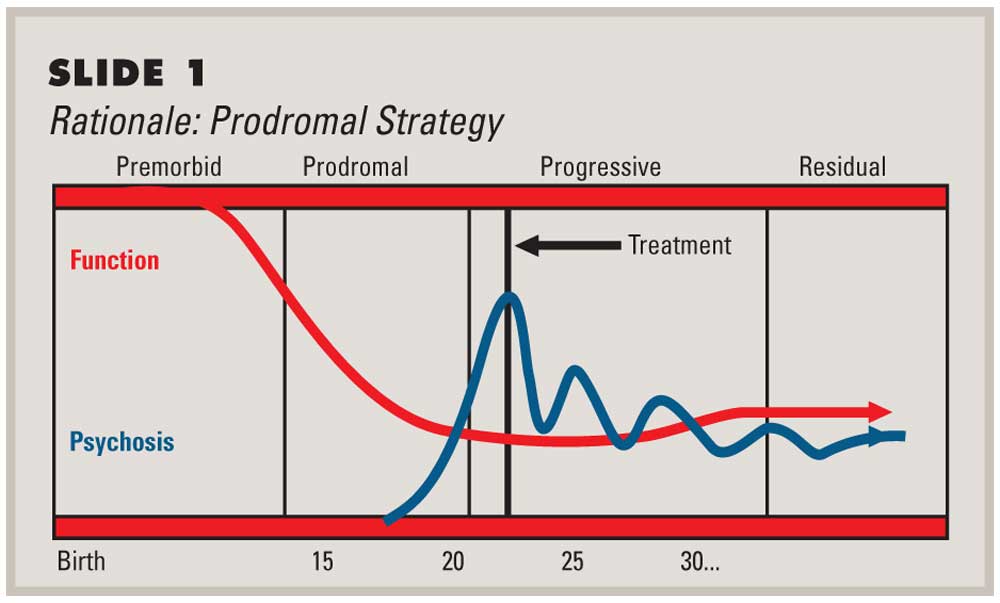
Prodromal phase: Schizophrenia usually starts with this phase, when symptoms are vague and easy to miss. They are often the same as symptoms of other mental health problems, such as depression or other anxiety disorders.
Positive symptoms of schizophrenia, such as hallucinations and delusions, make treatment seem more urgent, and they can often be effectively treated with antipsychotic drugs. But negative symptoms are the main reason patients with schizophrenia cannot live independently, hold jobs, establish personal relationships, and manage everyday social situations. These symptoms are also the ones that trouble them most. Surveys find that “the chief concerns of schizophrenic people are difficulty in concentrating, thinking, socializing, and enjoying life” (Shtasel et al., 1992). Schizophrenia’s negative symptoms have traditionally been viewed as treatment-resistant, but recent studies show that they do respond to pharmacologic and social interventions.
In 2003, Moller et al. published a systematic review of previous literature focusing on the pharmacological treatment of the negative symptoms of schizophrenia. Their purpose was to contrast and combine results from studies (published between 1995 and 2002) that compared the efficacy of typical and atypical antipsychotics in the treatment of the negative symptoms of schizophrenia. Their results indicated that atypical antipsychotics, such as clozapine and olanzapine are more effective in treating negative symptoms of acute schizophrenic episodes than typical antipsychotics such as haloperidol. As evident in the findings of Moller et al.’s meta-analysis, clinical studies in patients with schizophrenia suggest that second generation neuroleptics are more effective than typical neuroleptics in reducing negative symptoms such as anhedonia and flat affect.
So, here the question is: What makes atypical antipsychotics more effective?
Previous literature suggests that dysfunction of the ventral striatum, thus, the dopaminergic reward system may contribute to the development and persistence of negative symptoms in schizophrenia (Heinz et al., 1998). According to this hypothesis, atypical antipsychotics are more effective in treating negative symptoms because they significantly reverse the blunting of ventral striatal activation.
Juckel et al.’s 2006 fMRI study aimed to test this hypothesis by assessing ventral striatum activation in 10 schizophrenics taking typical antipsychotics, 10 schizophrenics taking atypical antipsychotics and 10 healthy control subjects during an incentive monetary task. Their results indicated that healthy control subjects and patients taking atypical antipsychotics showed a significant increase in BOLD response in their ventral striatum during anticipation of potential monetary gain, while patients taking typical antipsychotics did not.
They also found that decrease in the activation of the ventral striatum was correlated with the severity of negative symptoms. Less striatum activation meant more severe negative symptoms. In summary, significant blunting of ventral striatal activation was not observed in patients treated with atypical neuroleptics, which reflects the improved efficacy of these drugs in treating negative symptoms.
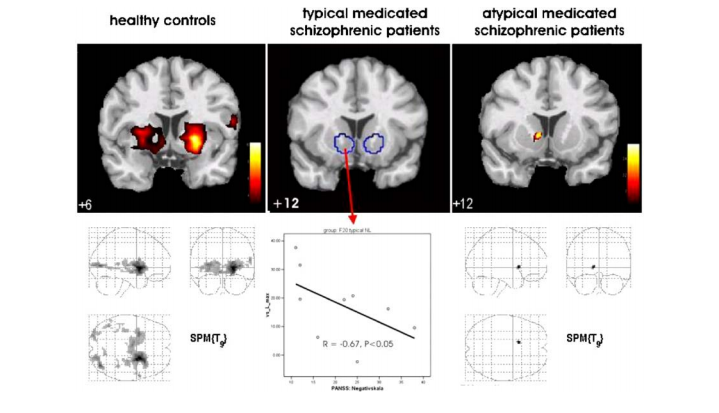
Ventral striatum activation during an incentive monetary task: healthy controls > atypical medicated schizophrenic patients > typical medicated schizophrenic patients
To conclude, negative symptoms represent an important treatment target in schizophrenia. In recent years, our understanding of these symptoms has benefited greatly from the adoption of methods from the field of affective neuroscience. Scientific findings suggest a role for second-generation antipsychotics in reducing the debilitating effects of negative symptoms, but we have yet to find the ultimate cure for emotion deficits in schizophrenia. Demystification of schizophrenia, along with recent insights from neuroscience and neuropsychology, gives new hope for finding more effective treatments for those suffering from this illness, who were once thought to be possessed by demons and were feared, tormented or locked up forever.
Sources:
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. (2013). Washington, D.C: American Psychiatric Association.
- Shtasel DL, Gur RE, Gallacher F, Heimberg C, Cannon TD, Gur RC. Phenomenology and functioning in first episode schizophrenia. Schizophrenia Bulletin 1992;18:449-462.
- Moller HJ. Management of the negative symptoms of schizophrenia: new treatment options. CNS Drugs 2003;17: 793:823.
- Juckel G, Schlagenhauf F, Koslowski M, Foliniv D, Wustenberg T, Villringer A, Knutson B, Kienast T, Gallinat J, Wrase J, Heinz A. Dysfunction of ventral striatal reward prediction in schziophrenic patients treated with typical, not atypical, neuroleptics. Psychopharmacology 2006; 187: 222-28.
- Fig 1: http://www.thementalelf.net/wp-content/uploads/2013/05/shutterstock_81409651.jpg
- Fig 2: http://www.cnsspectrums.com/userdocs/articleimages/86/1007Perk1big.jpg
- Fig 4: Moller HJ. Management of the negative symptoms of schizophrenia: new treatment options. CNS Drugs 2003;17: 793:823.