SHORT COMMUNICATION
Dr. Morn Ingbrew1
1Sunnyside University, Department of Science™
Abstract:
Temperature screening was initially used during the COVID-19 pandemic to prevent the entry of potentially infectious individuals into public places, either via infrared thermometers at the door, or through attestation that one is not running a fever. Despite overwhelming evidence that it doesn’t matter (plenty of people with COVID-19 do not run a fever), this is still somehow the standard for weeding out, well, a random assortment of people. Most households have access to an oral thermometer – be it of the digital or staggeringly archaic mercury variety (how are those still around?) – that can be used for screening, yet little attention has been paid to the potential effects of food or drink on oral temperature during these times. The results of this case study suggest that more attention to this topic is warranted if temperature is to be used as a non-laughable screening tool during a global pandemic.
Introduction:
In December of 2019, a number of pneumonia cases were reported in Wuhan, China. These were later found to be caused by a novel strain of coronavirus, termed SARS-CoV-2 [1]. SARS-CoV-2 is closely related to the viruses that caused the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) pandemics in 2003 and 2012, respectively [2]. Patients with these viruses often, but not always (because that would be too strong of a statement), present with “cold-like” symptoms, loss of taste and smell, and a fever.
Identifying individuals with fever was considered a priority at the beginning of the pandemic. Infrared thermography allows for rapid detection (less than or equal to 1 second) of the temperature of an individual, making it an excellent candidate for screening moving populations of people. Furthermore, most households have access to an oral thermometer (seriously, who greenlit the mercury ones?) that could be used for at-home screening prior to leaving the house each day, if one were disciplined enough to do so daily. Some studies have shown high levels of sensitivity and specificity from infrared thermometers [3]. Other research from previous pandemics suggests that the risk of missing febrile individuals using infrared thermometers could be up to 85%, so it’s unclear why this was a priority at all [4].
Since SARS-CoV-2 can spread asymptomatically (the incidence of asymptomatic individuals ranges from 1.6% to 56.5% in the literature, a terribly useless estimate), I cannot stress enough how likely it is that many potential spreaders will be missed using this strategy, regardless of whether the thermometer is a standard oral thermometer or an infrared doo-hickey.
Nevertheless, I embarked on a journey to conduct the most important experiment of our time, a study of many volunteers (n=1) to determine how the measurement of body temperature changes after drinking a beverage.
Methods:
Body temperature measurement
Body temperature was measured using a standard drugstore oral thermometer (BD Consumer Healthcare Model #403001) in ˚F (because who cares about metric anyways?).
Hot Coffee
8 ounces (237 mL) of coffee (Green Mountain Nantucket Blend) was brewed using a Keurig (192˚F brewing temperature). 1 teaspoon (4 g) of sugar and 2 ounces (60 mL) of lactose free whole milk (Hood®) was added prior to consumption. Baseline body temperature was measured prior to brewing the coffee. The coffee was brewed and imbibed within 21 minutes. The coffee was the test subject’s first oral intake of the day. Body temperature was measured immediately after the coffee was finished (t = 0 min) and every 5 minutes thereafter for 30 minutes. The test subject remained on the couch and did not move significantly during this time period.
Cold Coffee
The test subject (okay it’s me, I am the test subject) measured their baseline body temperature before preparing 8 ounces of cold coffee at 4˚C from a coffee stock and milk (both stored in the refrigerator). The coffee was imbibed within 21 minutes. The coffee was the test subject’s first oral intake of the day. Body temperature was measured immediately after the coffee was finished (t = 0 min) and every 5 minutes thereafter for 30 minutes. The test subject remained on the couch and did not move significantly during this time period.
Statistical Analysis
Data were analyzed in GraphPad Prism 9.0.1 by ordinary one-way ANOVA followed by the Holm- Šídák test to correct for multiple comparisons, because that one sounded the fanciest. All comparisons were made to the baseline temperature.
Results:
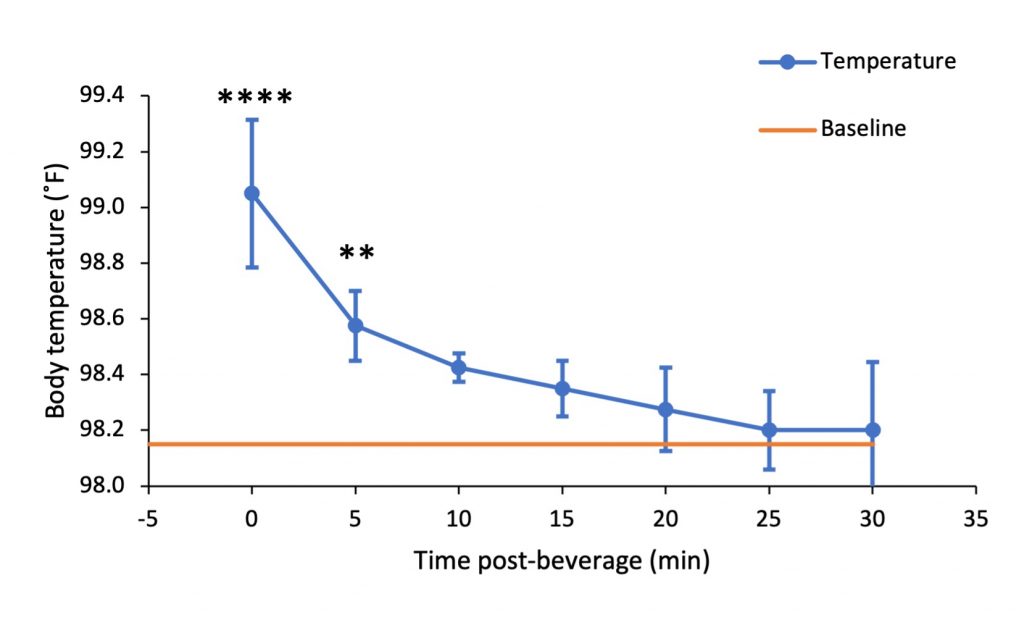
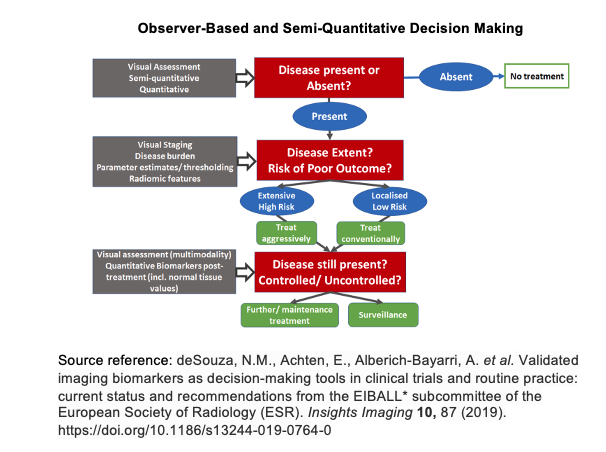
After drinking 8 ounces of a hot beverage, a sharp increase in body temperature was observed in the subject. However, this increase did not reach the level of a “fever” which the United States Centers for Disease Control considers 100.4˚F (38˚C) [5]. By 10 minutes post-beverage, the difference in temperature from baseline was no longer significant.
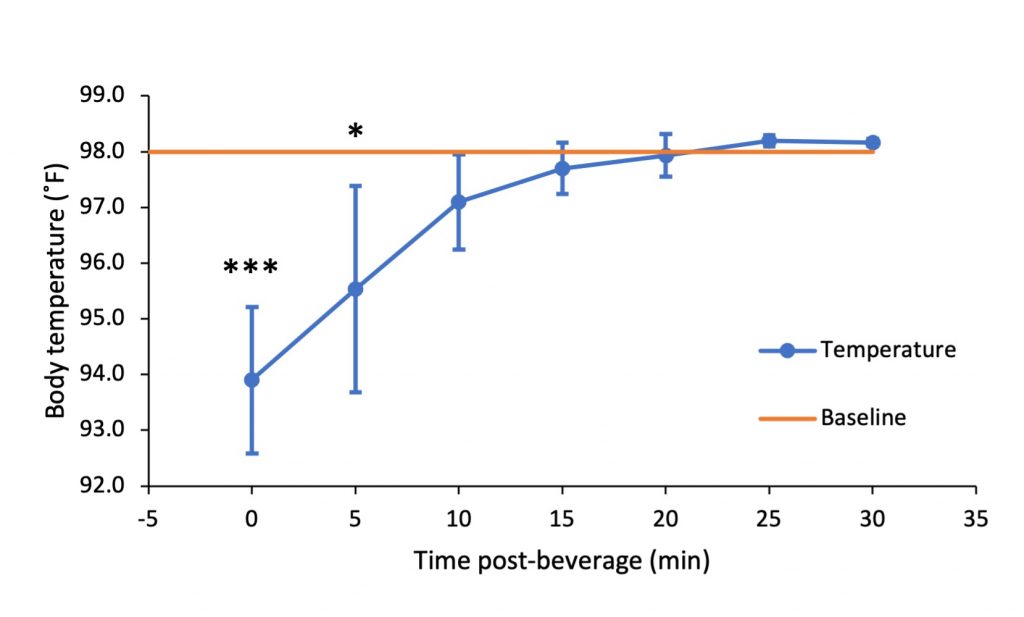
After drinking 8 ounces of a cold beverage, a large decrease in body temperature was observed. Similar to what was observed in the hot beverage trial, the subject’s body temperature was no longer significantly different from the baseline temperature after 10 minutes.
Discussion:
This case study demonstrates how measured body temperature changes with oral intake of beverages. As expected, hot beverages increased measured temperature of the subject and cold beverages decreased it. However, I had to show it, or people wouldn’t think I had done the work. Interestingly, the body temperature normalized within 10 minutes in contrast to some reports which showed that it took 15-20 minutes to normalize body temperature [6, 7].
Self-reported fevers are likely to rely on oral temperature readings (I have no evidence of this, but I feel strongly that it is the case). This study shows, however, that care must be taken when using oral thermometers for screening fevers, since the measured body temperature can fluctuate with oral intake. When screening for fevers in the context of a global pandemic, it is arguably more concerning to potentially miss an individual whose temperature has been artificially lowered by consumption of a cold beverage than to “catch” an individual whose temperature has been artificially elevated by a hot one. These results suggest waiting at least 10 minutes after drinking to measure body temperature orally.
While this study is limited to temperature measured orally, it is not difficult to extrapolate the results to temperatures measured by infrared thermometers. A study by Jay et al. in 2007 showed that mean skin temperature, measured by thermocouples at 12 sites on the body, increases with exercise, suggesting that a habituation period might be warranted for any febrile screening procedures to ensure accurate temperature measurements, regardless of mode of measurement [8].
Acknowledgements:
No one, because no one funded the author for this research. They are an independent researcher who doesn’t need a funding agency anyway.
I’m just kidding. Please fund me.
References:
[1] Cucinotta D and Vanelli M. (2020) WHO declares COVID-19 a pandemic. Acta Biomed 91(1):157-160.
[2] Yang Y, Peng F, Wang R, et al. (2020) The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J Autoimmun 109:102434.
[3] Tay MR, Low YL, Zhao X, et al. (2015) Comparison of Infrared Thermal Detection Systems for mass fever screening in a tropical healthcare setting. Public Health 129:1471-1478.
[4] Bitar D, Goubar A, and Desenclos JC. (2009) International travels and fever screening during epidemics: a literature review on the effectiveness and potential use of non-contact infrared thermometers. Eurosurveillance 14(6):19115.
[5] U.S. Department of Health & Human Services. Accessed 23 Feb 2021. https://www.cdc.gov/quarantine/air/reporting-deaths-illness/definitions-symptoms-reportable-illnesses.html
[6] Quatrara F, Coffman J, Jenkins T, et al. (2007) The effect of respiratory rate and ingestion of hot and cold beverages on the accuracy of oral temperatures measured by electronic thermometers. MedSurg Nurs 16(2):105-108.
[7] Mousa O, Al Saleh K, Al Subaie, et al. (2018) Effects of cold and hot beverage on oral temperature. IOSR J Nurs Health Sci 7(4):24-27.
[8] Jay O, Reardon FD, Webb P, et al. (2007) Estimating changes in mean body temperature for humans during exercise using core and skin temperatures is inaccurate even with a correction factor. J Appl Physiol 103:443-451.