Clinical Teaching Tip: Feedback that Creates Change

By Carie Cardamone, PhD, Associate Director of STEM & Professional Schools, Center for the Enhancement of Learning and Teaching
Feedback is one of the most powerful learning tools in a teaching clinic. However, in a busy clinical environment, where time is limited and settings are diverse, feedback can be a source of discomfort and stress for both the staff and learners. Staff must balance the needs of maintaining professional standards, the self-esteem and learning of the students, and the rights and safety of patients. Typically, students experience variable feedback techniques, as well as differing quantity and quality of feedback throughout their time in the clinic. This can result in students perceiving a lack of helpful feedback. From the faculty side, it is easy to become overwhelmed by the burden of providing feedback, and staff may have concerns about the dynamics and reception of the feedback they provide.
The most effective feedback improves a student’s performance and knowledge while increasing their capacity to make judgements about their own work. Rather than a one-way transmission of information from a knowledgeable person to a learner, effective feedback is a process by which a learner deepens their understanding of the similarities and differences between their performance and the standards to which they will be held as professionals. Ultimately, feedback should enable the learner to change and grow.
To provide constructive feedback consider the following:
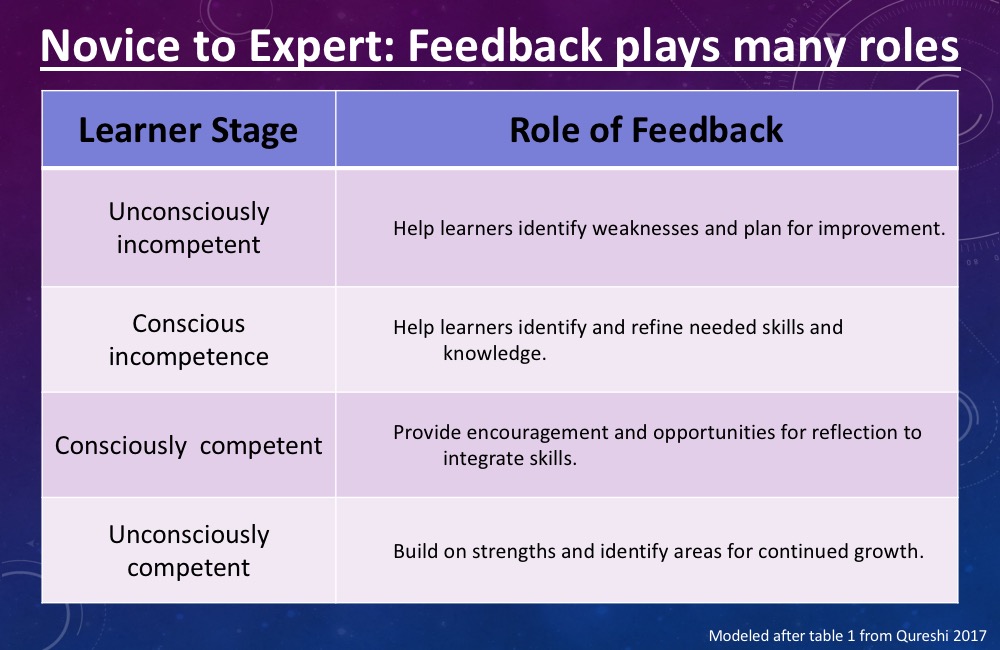
Start with the Learner: The learner must be able to understand and act on the feedback provided. Recognize that each student’s context is different, and carefully consider the assumptions that you are making. Assumptions about a student’s background can negatively influence their ability to recognize the usefulness of the information provided. Adapt your feedback to align with the learner’s location along the continuum from Novice to Expert (see Table 1). Start a feedback conversation by inquiring about the learner’s own perceptions of their performance, and their ideas for improvement, then relate any feedback provided to the learner’s goals.
Make Observations not Judgements: Target modifiable behavior with objective observations. Evaluative feedback can trigger negative emotions, making it more difficult for the student to internalize and act on the information provided. Frame the feedback as an opportunity for self-improvement by modeling a growth mindset and allowing the student to articulate strategies for improvement.
Be Timely & Specific: Frequent focused feedback carries a greater impact than delayed evaluative feedback. This is most important for procedural skills, where immediate feedback can be immediately implemented in practice. When providing feedback, highlight a specific aspect of a performance to accentuate or change. Broad feedback, such as unconditional praise, is often ignored as there are no concrete ties to the learners actions. When necessary, call the student aside for a moment to give feedback away from the patient or the group.
Limit feedback to key points & check on their reception: When feedback is complex, such as a long list of things to change, the learner often loses the main messages. As a result, changes to the student knowledge or practice can be negatively impacted. After sharing a couple of key pieces of feedback, ask the student for questions that they might have, their perspective on what they’ve heard, or for suggestions for a plan to improve their performance. Before ending the conversation, ensure that the feedback is accepted and that the student has a concrete plan for improvement.
Embedding a culture of feedback can provide a more relaxed environment, and lead to better student learning and patient care. To foster the feedback culture – help set expectations for students to actively seek and expect feedback, and for faculty collaborate to provide consistent feedback mechanisms across the clinic floor.
References & Further Reading
- Giving Feedback in Clinical Settings by Cantillon & Sargeant, 2008, in Teaching Rounds
- State of the Science in Health Professional Education: Effective Feedback, Archer, 2009, in Medical Education
- Clarifying Students’ Feedback-Seeking Behaviour in Clinical Clerkships by Bok et al., 2013, in Medical Education
- Seeking a Different Angle on Feedback in Clinical Education: The Learner as Seeker, Judge and User of Performance Information by Moloy & Boud, 2013, in Medical Education
- Initiatives to Improve Feedback Culture in the Final Year of a Veterinary Program, Warman, 2014, in Journal of Veterinary Medical Education
- Feedback: ensuring that it leads to enhanced learning by Boud, 2015, in Clinical Teacher
- Giving effective feedback in medical education by Qureshi, 2017, in The Obstetrician & Gynaecologist